Cell Res:中科院杨巍维研究组揭示癌细胞适应氧化应激的重要机制
2017-01-04 佚名 生物谷
近日,中科院上海生命科学研究院生化细胞所杨巍维研究组在国际学术期刊Cell Research上发表了一项最新研究进展,他们证实线粒体PKM2可通过稳定Bcl2调节氧化应激诱导的细胞凋亡。由于癌基因刺激、代谢活性增加和线粒体功能紊乱等因素,癌细胞的活性氧水平高于正常细胞。在持续的氧化应激情况下,癌细胞通过一系列机制得以适应,不仅激活ROS清除系统,也会抑制细胞凋亡。许多研究表明癌细胞的这种适应性会

近日,中科院上海生命科学研究院生化细胞所杨巍维研究组在国际学术期刊Cell Research上发表了一项最新研究进展,他们证实线粒体PKM2可通过稳定Bcl2调节氧化应激诱导的细胞凋亡。
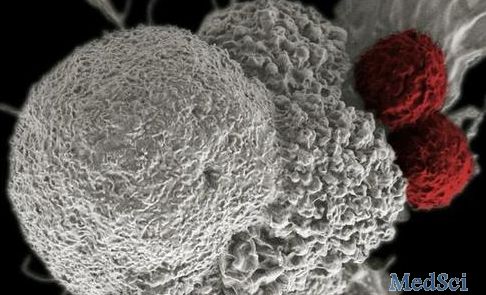
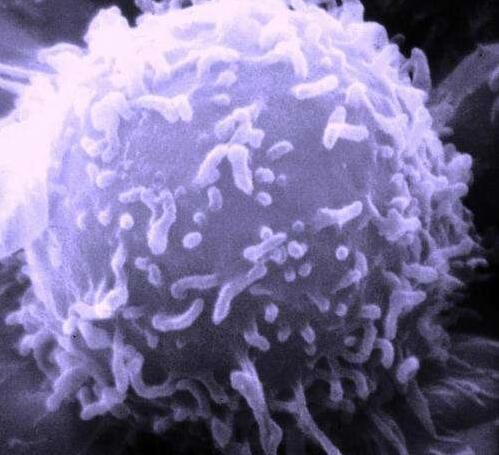
由于癌基因刺激、代谢活性增加和线粒体功能紊乱等因素,癌细胞的活性氧水平高于正常细胞。在持续的氧化应激情况下,癌细胞通过一系列机制得以适应,不仅激活ROS清除系统,也会抑制细胞凋亡。许多研究表明癌细胞的这种适应性会促进恶性转化、转移和对抗癌药物的抵抗,因此理解ROS适应机制对于杀死癌细胞解决耐药问题是非常重要的。
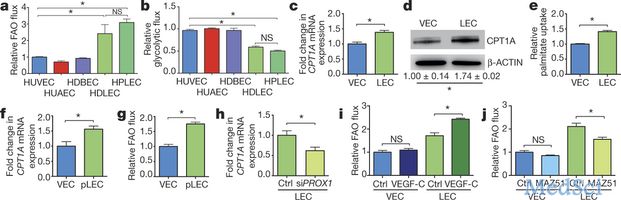
PKM2能够催化糖酵解的最后一步,对于肿瘤细胞增殖也非常重要。在这项研究中,研究人员发现PKM2在氧化应激条件下会转定位到线粒体,在线粒体与Bcl2结合并将其磷酸化。这种磷酸化修饰会阻止Bcl2与Cul3为基础的E3连接酶的结合,防止Bcl2的降解。研究人员还发现分子伴侣HSP90α1是PKM2发挥该功能所必需的一个分子,HSP90α1的ATP酶活性可引起PKM2发生构象变化,促进PKM2与Bcl2的结合。将野生型Bcl2替换为磷酸化缺陷的突变体会增加胶质瘤细胞对氧化应激诱导细胞凋亡的敏感性,并损伤原位移植模型中的脑肿瘤形成。
值得注意的是,单独合成PKM2与Bcl2结合的肽段能够破坏PKM2与Bcl2的相互结合促进Bcl2降解,损伤脑肿瘤生长。此外,Bcl2 T69磷酸化水平,构象改变的PKM2和Bcl2蛋白在人类胶质母细胞瘤患者标本中彼此关联,Bcl2 T69磷酸化水平和构象改变的PKM2还与胶质瘤恶性程度等级以及肿瘤预后相关。
这些结果揭示了癌细胞可以在氧化应激情况下通过定位在线粒体的PKM2与Bcl2之间的相互作用抑制细胞凋亡,表明PKM2在癌细胞对ROS的适应性中具有至关重要的作用,因此HSP90-PKM2-Bcl2可能是治疗胶质母细胞瘤的一个潜在靶点。
原始出处
Ji Liang1,2,3,*, Ruixiu Cao1,2,3,*, Xiongjun Wang1,2,3, Yajuan Zhang1,2,3, Pan Wang1,2,3, Hong Gao1,2,3, Chen Li1, Fan Yang4, Rong Zeng1, Ping Wei5, Dawei Li6, Wenfeng Li7 and Weiwei Yang.Mitochondrial PKM2 regulates oxidative stress-induced apoptosis by stabilizing Bcl2.Cell Res.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#中科院#
53
#CEL#
66
#Cell#
56
#癌细胞#
56
#应激#
65