CCR7预示SCC颈部淋巴结转移
2012-09-25 网络 网络
根据对60例成人患者的资料分析,趋化因子受体CCR7表达可预示口腔鳞状细胞癌(SCC)颈部淋巴结转移。 加州大学戴维斯分校的Levi G. Ledgerwood博士在美国耳鼻喉-头颈外科学会基金会(AAO-HNSF)2012年会上报告指出,SCC转移扩散较为常见,但其机理尚不清楚。近期研究集中于血流和外周组织T细胞进入淋巴道所必须的细胞表面分子—趋化因子受体CCR7。既往研究提示,CCR7
根据对60例成人患者的资料分析,趋化因子受体CCR7表达可预示口腔鳞状细胞癌(SCC)颈部淋巴结转移。
加州大学戴维斯分校的Levi G. Ledgerwood博士在美国耳鼻喉-头颈外科学会基金会(AAO-HNSF)2012年会上报告指出,SCC转移扩散较为常见,但其机理尚不清楚。近期研究集中于血流和外周组织T细胞进入淋巴道所必须的细胞表面分子—趋化因子受体CCR7。既往研究提示,CCR7可能在多种癌症淋巴结转移过程中扮演重要角色。

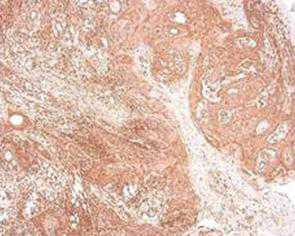
组织标本显示CCR7表达阳性
Ledgerwood博士及其同事考察了一家医院2006~2011年收治的60例口腔SCC手术切除患者的组织标本,其中包括30份转移患者和30份未转移患者的标本。每组男性患者均较多,未见组间人口统计学显著差异。淋巴结阳性和阴性患者各30例。
总体上,颈部转移患者CCR7表达率明显高于未转移者(P<0.001)。共计97%的淋巴结阳性患者CCR7表达阳性,但无颈部转移患者仅为43%。对转移患者淋巴结样本检查结果显示,所有30例淋巴结阳性患者均有CCR7表达。
组织标本显示CCR7表达阴性
研究者指出,尽管这项研究存在样本量较小的局限性,但结果表明CCR7可能在T细胞进入淋巴道的过程中发挥作用。此外,虽然这是一项初步研究,但仍提示CCR7是值得关注的潜在治疗靶点,并有助于预测肿瘤行为。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SCC#
101
#淋巴结#
70
#淋巴结转移#
80
#颈部#
75