JAMA:冠状动脉造影术后睾丸酮疗法与不良结局风险增高有关
2013-11-11 佚名 丁香园
在行冠状动脉造影术及低睾丸酮水平的男性群体中,睾丸酮的使用与死亡、心脏病发作、缺血性中风风险增高有关。这是一项由西南医学中心德克萨斯大学的Rebecca Vigen博士、Dallas及其同事进行的研究,研究结果在线发表于11月6日的《美国医学会杂志》(JAMA)上。【原文下载】 在过去十年内,睾丸酮治疗处方比例在美国显著增加。从2000年到2011年,睾丸酮每年的处方
在行冠状动脉造影术及低睾丸酮水平的男性群体中,睾丸酮的使用与死亡、心脏病发作、缺血性中风风险增高有关。这是一项由西南医学中心德克萨斯大学的Rebecca Vigen博士、Dallas及其同事进行的研究,研究结果在线发表于11月6日的《美国医学会杂志》(JAMA)上。【原文下载】
在过去十年内,睾丸酮治疗处方比例在美国显著增加。从2000年到2011年,睾丸酮每年的处方量以5倍以上的速度增长,2011年达到530万份处方,市场份额达16亿美元。专业社团指导原则推荐睾丸酮用于治疗症状性睾丸酮缺乏的患者。除了改善性功能和骨矿物质密度,以及增加组织非脂肪量和强度,睾丸酮治疗还能够改善脂质分布情况和胰岛素抵抗,同时增加应激试验期间ST段压低时间(心电图上有临床益处的一个发现)。但是,最近一项关于睾丸酮治疗高心血管疾病患病率男性的随机临床试验由于不良心血管事件过早中断,这引起了人们对睾丸酮治疗安全性的担忧。因此,Rebecca Vigen博士等对睾丸酮疗法与男性退伍军人全因死亡、心肌梗塞(MI;心脏病发作)和中风的相关性,以及这种相关性是否受潜在冠状动脉疾病(CAD)的改变进行了研究。
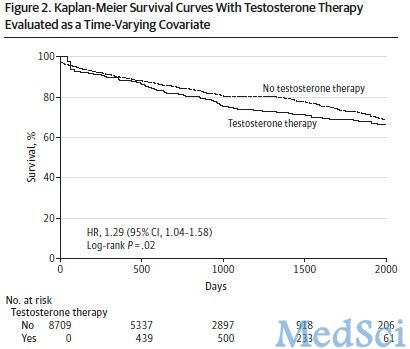
该项研究纳入退伍军人事务部(VA)系统中2005年-2011年的8,709名行冠状动脉造影术及低睾丸酮水平(<300ng/dL)男性。该组人群并发症程度较严重,包括前期心脏病发作病史、糖尿病或CAD.在8,709名患者中,1,223名患者(14.0%)于造影术后中位时间531天开始接受睾丸酮治疗。平均随访时间约2年,3.5个月。主要测量结果包括全因死亡、心脏病发作和缺血性中风。
结果显示,无睾丸酮治疗组患者(平均年龄64岁)冠状动脉造影术后3年发生不良事件的比例为19.9%,而睾丸酮治疗组为25.7%(平均年龄61岁),绝对风险差异为5.8%.尽管对其它可能解释这种差异性的影响因素加以说明,使用睾丸酮治疗还是与不良结局有关,并且这一结果在CAD和非CAD患者中是一致的。使用睾丸酮治疗增加的不良结局风险与危险因素或二级预防药物使用比例的差异无关,因为两组患者血压、低密度脂蛋白水平和二级预防药物使用相似。
这些研究发现引起人们对睾丸酮疗法潜在安全性的担忧。因此,将来需要进行一些研究(包括随机对照临床试验),以便正确描述睾丸酮治疗有并发症男性的潜在风险特点。
原文出处:
Vigen R, O'Donnell CI, Barón AE, Grunwald GK, Maddox TM, Bradley SM, Barqawi A, Woning G, Wierman ME, Plomondon ME, Rumsfeld JS, Ho PM.Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels.JAMA. 2013 Nov 6;310(17):1829-36. doi: 10.1001/jama.2013.280386.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#造影术#
59
#睾丸#
43
#冠状动脉造影#
58
#造影#
70
#增高#
57
#增高#
44