EuroPCR 2015:[高润霖院士]阜外介入治疗左主干病变三年死亡率仅4.2%
2015-06-04 yiwen 医师报
5月19-22日,欧洲血运重建大会(EuroPCR)在法国巴黎隆重召开,全球1.2万名学者及医生云集在此,共享这一全球介入盛会。高润霖院士在大会上介绍了阜外心血管病医院左主干病变PCI治疗的3年随访结果。 高院士指出,PCI治疗左主干病变具有较低的支架内血栓形成、血运重建和死亡发生率,但应避免用于SYTAX评分>32分的患者。而且,术者经验对临床预后有很大影响,应给予高度重视。 该研究纳
5月19-22日,欧洲血运重建大会(EuroPCR)在法国巴黎隆重召开,全球1.2万名学者及医生云集在此,共享这一全球介入盛会。高润霖院士在大会上介绍了阜外心血管病医院左主干病变PCI治疗的3年随访结果。
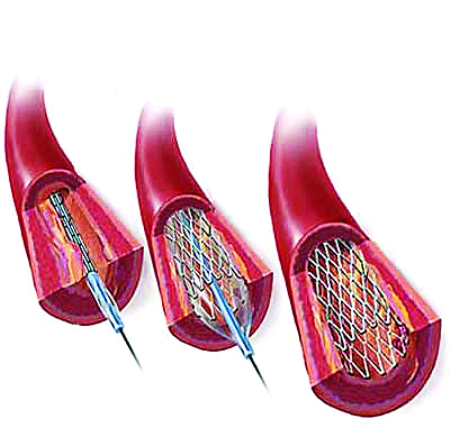
高院士指出,PCI治疗左主干病变具有较低的支架内血栓形成、血运重建和死亡发生率,但应避免用于SYTAX评分>32分的患者。而且,术者经验对临床预后有很大影响,应给予高度重视。
该研究纳入2004-2011年,在阜外医院接受左主干PCI的1948例患者。左主干PCI占总PCI例数的4%左右。其中,末端分叉病变超过80%,合并三支病变接近40%;Syntax评分为(24.0±7.1)分。
结果显示,30 d和3年全因死亡率分别为1.0%和4.2%;靶血管血运重建发生率分别为0.9%和6.2%;支架内血栓形成发生率分别为0.6%和1.7%。
与经验不丰富的医生相比,由经验丰富的医生进行左主干介入治疗,所完成病例的Syntax评分更高,合并三支病变的比例更高,30 d(0.6% vs 2.1%)和3年(3.8% vs 5.4%)全因死亡率更低,3年死亡、卒中和心肌梗死复合终点发生率也更低(9.1%vs 11.1%)。
高院士还比较了Syntax评分和SyntaxⅡ评分对预后的影响。
Syntax评分分别为>32分、23~32分和≤22分的患者,3年死亡率分别为8.2%、4.2%和3.2%,死亡、卒中和心肌梗死复合终点发生率分别为15.6%、11.2%和6.4%。
SyntaxⅡ评分分别为>28分、21~28分和≤21分的患者,3年死亡率分别为7.3%、4.0%和1.6%,死亡、卒中和心肌梗死复合终点发生率分别为14.0%、10.2%和5.2%。
此外,高润霖院士还比较了冠脉旁路移植术(CABG)与PCI治疗左主干病变的结果。其中包括2917例CABG患者,1528例PCI患者。
与CABG相比,PCI的事件发生率仍略高(3.8%vs 2.5%),特别是Syntax评分≥33分的患者,PCI治疗的3年全因死亡率高达7.8%,显著高于CABG组(2.4%);而Syntax评分≤32分的患者,PCI和CABG的3年全因死亡率接近(3.2%vs 2.7%)。

图1 不同Syntax评分患者行血运重建的3年全因死亡率
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了啊
77
#左主干#
66
#高润霖#
78
#EuroPCR#
70
很好的比较和研究!
157
#PCR#
57