Blood:肝素诱导性血小板减少症的早期确诊方法!
2020-09-17 QQY MedSci原创
肝素诱导性血小板减少症(HIT)是一种危及生命的、促血栓形成的、抗体介导性疾病。为了最大限度地提高康复的可能性,早期准确诊断至关重要。
广泛使用的HIT检验,如血小板因子4-肝素ELISA 缺乏特异性,而被视作“金标准”的C14标记的血清素释放试验(SRA)因为只能通过参考实验室获得,在早期患者管理中的应用价值有限。
近期研究表明,“致病性”HIT抗体可选择性地激活PF4处理的血小板;而一种技术上更简单的检测方法——PF4依赖的P-选择素表达分析(PEA),可能会提供一种快速且准确检测。
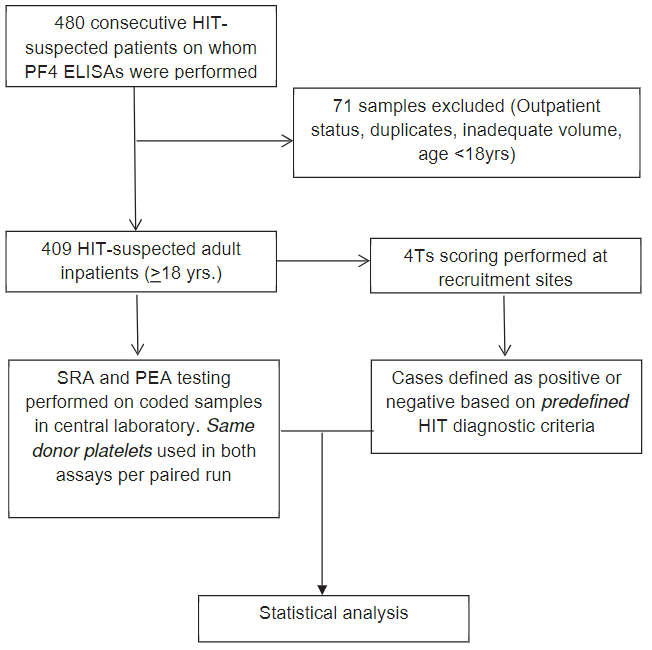
根据4Ts评分和HIT ELISA结果结合的预定义标准,将409名疑似HIT的成人分为疾病阳性、阴性或不确定。被划分为“HIT-不确定”的患者在初步分析中被认为是疾病阴性的,在敏感性分析中被认为是疾病阳性。
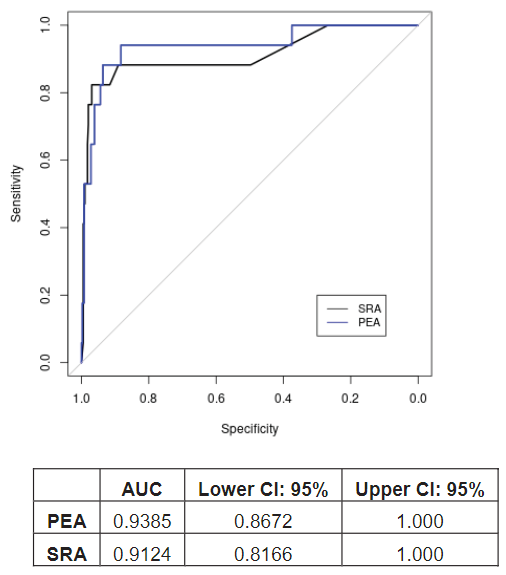
采用受试者操作特征曲线统计,比较PEA和SRA诊断HIT患者的能力。使用这些预先定义的标准,PEA的诊断准确率较高(曲线下面积[AUC]为0.94;95%CI 0.87~1.0),与SRA的相似(0.91;0.82~1.0)。在敏感性分析中,PEA和SRA的AUC也相似,分别为0.88(0.78~0.98)和0.86(0.77~0.96)。
综上所述,PEA是一种技术简单的非放射性检测方法,与SRA相比,它使用的血小板减少了约20倍,对HIT的诊断具有很高的准确性。PEA的广泛应用可能有助于及时和更有效地处理疑似HIT患者。
原始出处:
Bethany T Samuelson Bannow, et al. A prospective, blinded study of a PF4-dependent assay for HIT diagnosis. Blood. September 8, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#诱导性#
79
#肝素诱导性血小板减少症#
70
不错
116
#血小板减少#
102
不错的结果
109
学习了,谢谢分享
131
学习学习
118
很好
129