Nature:新发现的抗体有望开发新药治疗更年期骨质疏松和肥胖!
2017-05-27 佚名 Nature 自然科研
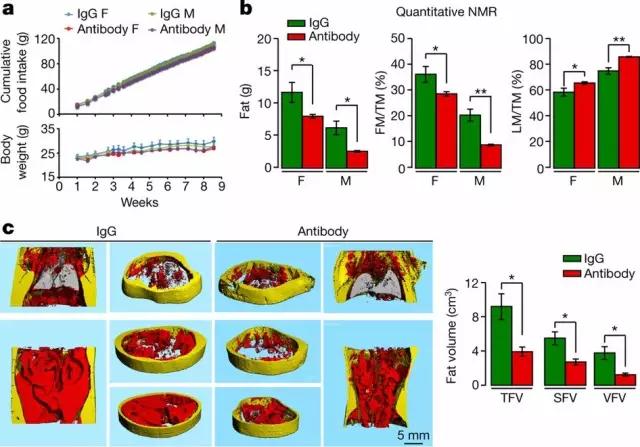
本周《自然》在线发表的一篇论文Blocking FSH induces thermogenic adipose tissue and reduces body fat报告了一种新发现的抗体,在更年期模型小鼠身上进行的试验表明,它或有助于增加骨量,减少体脂。若要确定这些发现是否可以转化至人类身上,还需要进行进一步的研究。不过,本研究有望推动开发单一药物,帮助治疗更年期后骨质疏松症和体重增加情况,以及
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
68
#新发现#
56
#骨质#
53
努力学习!有用的
74
学习一下很不错
85
学习了谢谢分享
96