袁良喜:下肢动脉硬化闭塞症诊治指南解读——间歇性跛行的治疗
2015-10-12 MedSci MedSci原创
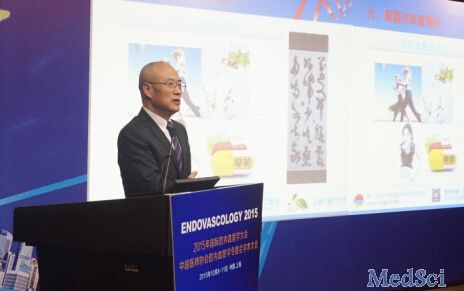
在2015年国际腔内血管学大会上,来自长海医院血管外科的袁良喜博士为我们解读了下肢动脉硬化闭塞症诊治指南中关于间歇性跛行的治疗。 间歇性跛行的治疗流程 保守治疗(控制危险因素、运动治疗、药物治疗3-6个月),效果良好则随访;疗效不佳,影像学可见病变,要考虑是否适合腔内治疗,若不适合则行传统外科手术治疗。 间歇性跛行的运动和康复治疗 运动治疗必须在专业指导下进
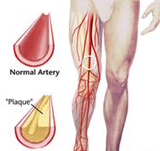
在2015年国际腔内血管学大会上,来自长海医院血管外科的袁良喜博士为我们解读了下肢动脉硬化闭塞症诊治指南中关于间歇性跛行的治疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











非常好!感谢感谢!
121
#间歇性#
69
#下肢动脉硬化闭塞症#
95
#下肢动脉#
70
#动脉硬化闭塞症#
76
赞一个~
169
非常感谢~
156
感谢分享
173
为了积分我也是拼了~
168
#间歇性跛行#
100