Clinica Chimica Acta:使用LC-MS/MS方法在女性月经周期、绝经后女性和男性中确定雌二醇参考区间
2019-09-21 gladiator MedSci原创
为了优化医疗决策,需要对不同年龄和性别的雌二醇的参考区间进行考虑。本研究的目的是用一种高精度、可跟踪的<span lang="EN-US" style="font-size:12.0pt;mso-bidi-font-size:14.0pt;font-family:"Calibri","sans-serif"; mso-fareast-font-family
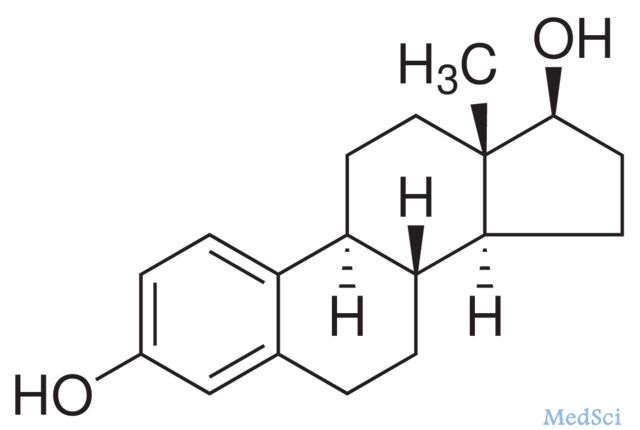
为了优化医疗决策,需要对不同年龄和性别的雌二醇的参考区间进行考虑。本研究的目的是用一种高精度、可跟踪的LC-MS/MS方法建立参考区间,并与文献中的参考区间进行比较。
研究人员对30例健康绝经前妇女月经周期中每日血清雌二醇水平,以及64例男性和33例绝经后妇女血清雌二醇水平进行测量。通过与CDC参考方法的比较,验证了LC-MS/MS方法的准确性。
研究显示LC-MS/MS方法可以与参考方法比较。在早期卵泡期(天-15到-6)雌二醇参考间隔为31-771皮摩尔/ L;在晚卵泡期(天-5〜-1)104-1742皮摩尔/ L; LH峰(第0天)275-2864皮摩尔/ L期间;在早期黄体期(天1至4)95-1188皮摩尔/ L;中期期间黄体期(天5至9)151-1941皮摩尔/ L;晚黄体期(天+10至+14)39-1769皮摩尔/ L。男性的参考间隔为12-136 pmol
/ L,而绝经后妇女<26皮摩尔/ L。
研究表明,本研究建立的雌二醇参考区间可用于所有可追溯的LC-MS/MS方法。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CTA#
57
#绝经#
56
#雌二醇#
124
#月经#
59
#绝经后女性#
101
#参考区间#
75
#绝经后#
66