Am J Cardiol:CRP升高示易损斑块不稳定性
2014-05-22 高晓方 译 医学论坛网
美国一项研究表明,在C反应蛋白(CRP)水平极高的急性冠脉综合征(ACS)后患者中,非罪犯病变(NCL)相关性严重不良心脏事件发生率较高可能反映了高危NCL更大程度的不稳定性。论文于5月19日在线发表于《美国心脏病学杂志》(Am J Cardiol)。 此项研究共纳入697例接受经皮冠脉介入(PCI)治疗的ACS患者,并对其进行为期3年随访。于患者就诊、1个月和6个月时测定CRP水平,并将其分类
美国一项研究表明,在C反应蛋白(CRP)水平极高的急性冠脉综合征(ACS)后患者中,非罪犯病变(NCL)相关性严重不良心脏事件发生率较高可能反映了高危NCL更大程度的不稳定性。论文于5月19日在线发表于《美国心脏病学杂志》(Am J Cardiol)。【原文下载】
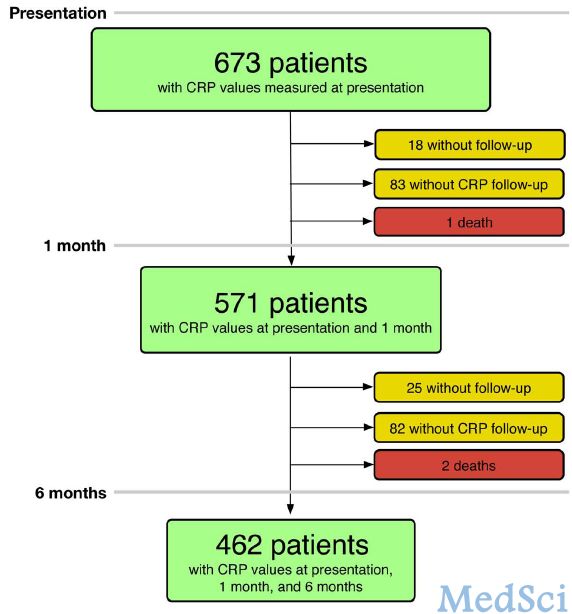
此项研究共纳入697例接受经皮冠脉介入(PCI)治疗的ACS患者,并对其进行为期3年随访。于患者就诊、1个月和6个月时测定CRP水平,并将其分类为正常(<3 mg/L)、升高(3~10 mg/L)或极高(>10 mg/L)三组。评估CRP与NCL的相互作用。
结果显示,各时间点CRP水平升高患者均未伴有更多的高危NCL。然而,与6个月时CRP水平正常者相比,在CRP水平极高患者中未经治疗的高危NCL更有可能导致后续严重不良心脏事件(MACE)。6个月时CRP水平极高患者后续NCL相关性MACE发生率较高(19.0%对7.2%,P=0.039)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cardiol#
52
#稳定性#
56
炎症与斑块不稳定的相关性又有了新证据
152
炎症与斑块不稳定的相关性又有了新证据
164
#CRP#
47
#斑块#
64