Cell:邹伟平教授揭秘肿瘤免疫与化疗关系
2016-05-04 生物谷 生物谷
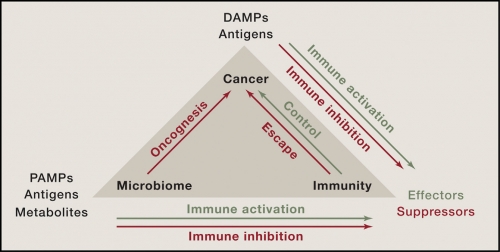
成纤维细胞会减少癌细胞内的铂含量,导致化疗药物抵抗 成纤维细胞释放的谷胱甘肽和半胱氨酸会促进癌细胞对铂的抵抗 T细胞可以改变成纤维细胞的谷胱甘肽和半胱氨酸代谢,削弱成纤维细胞介导的癌细胞对化疗药物的抵抗 成纤维细胞和CD8+T细胞共同左右了病人对化疗药物的应答 近日,来自美国密歇根大学的华人科学家邹伟平领导

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
63
#Cell#
65
现在医疗的趋势
152
做研究也很好
230
真的不错
174
学习了,很好的
155