TAG: 补充铁是否可以增加抗肿瘤坏死因子-α药物治疗炎性肠病患者疗效?
2020-10-17 网络 网络
炎性肠病(IBD)是一种慢性炎性疾病,其主要形式为溃疡性结肠炎(UC)和克罗恩氏病(CD)。IBD的主要症状和体征在肠道。但是,肠外表现很常见。
炎性肠病(IBD)是一种慢性炎性疾病,其主要形式为溃疡性结肠炎(UC)和克罗恩氏病(CD)。IBD的主要症状和体征在肠道。但是,肠外表现很常见。贫血是IBD的常见肠外表现之一, IBD患者的贫血会显着增加医疗保健成本,并对生活质量产生负面影响。在IBD患者贫血的发病率约为20-30%,CD比UC患者更加常见。 IBD患者的贫血可能源于多种原因。最常见的是由出血和吸收障碍引起的铁缺乏症,由炎症引起的铁体内平衡障碍以及由骨髓抑制和吸收障碍引起的维生素B12和叶酸缺乏症。肿瘤坏死因子-α(TNF-α)抑制剂(英夫利昔单抗和阿达木单抗)是IBD患者的一线生物治疗方法,黏膜愈合是治疗慢性炎性疾病的关键。本项研究旨在评估补充铁对最初用抗TNF-α药物治疗的IBD患者的效果。
研究人员收集了一些开始抗TNF-α治疗的79名IBD患者的数据。将患者分为抗TNF-α组(n = 52)和补充铁的抗TNF-α 组(n = 27)。在基线(第0年)和1年后评估不同疗法对实验室参数,贫血患病率和疾病活动性的影响。

研究结果显示:两组患者的第0年和第1年之间的血红蛋白(Hb)水平均显着升高[抗TNF-α组为12.0±1.8–13.3±2.0 g / dL(p <0.001)和抗TNF-α和铁补充组为9.8±2.4–11.7±2.3 g / dL(p = 0.004)]。在严重贫血的IBD患者的亚组分析中, 与抗TNF-α组(9.3±9.3)相比,补铁增加了Hb水平的改善幅度(8.5±1.5-11.4±2.1 g / dL;p = 0.001)。与第0年相比,两组的疾病活动在1年时均显着改善。持续性贫血与基线时的严重贫血显着相关(p = 0.017)。
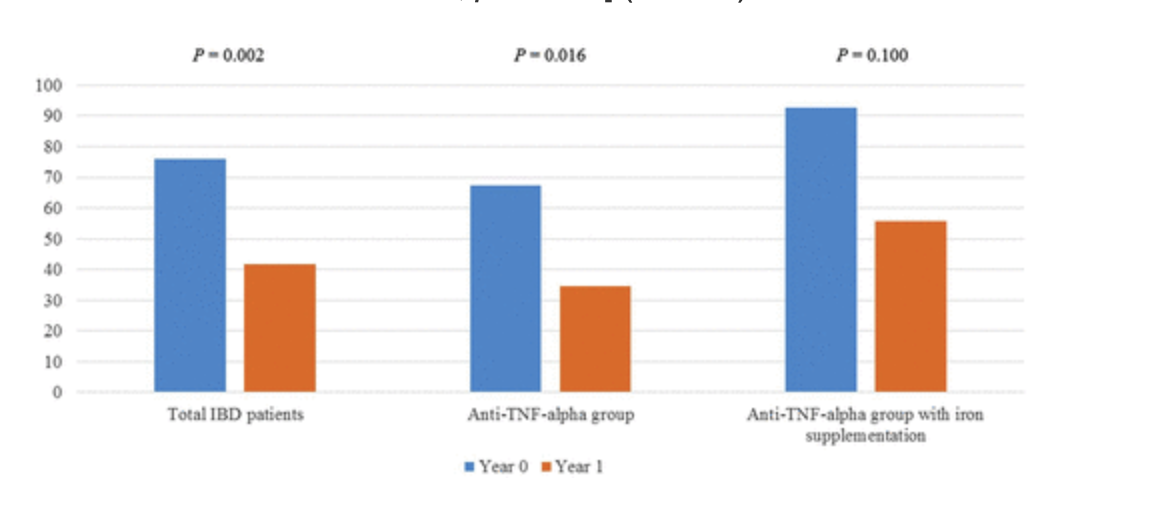
作者最后说道:在患有IBD的贫血患者中,抗TNF-α药物可以改善患者的贫血的状态,而与铁的补充无关。另外,补充铁可能对IBD严重贫血的患者有帮助。
原始出处:
Su Young Kim. Et al. Efficacy of iron supplementation in patients with inflammatory bowel disease treated with anti-tumor necrosis factor-alpha agents.Therapeutic Advances in Gastroenterology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#坏死#
59
#肿瘤坏死因子#
57
#抗肿瘤坏死因子#
0
#抗肿瘤坏死因子#
56
谢谢梅斯提供这么好的信息,学到很多
71