JCC:炎症性肠病患者的神经退行性疾病风险明显增加
2022-04-08 xuyihan MedSci原创
神经性退行可分为急性神经退行性疾病和慢性神经退行性疾病,前者主要包括脑缺血(CI)、脑损伤(BI)、癫痫;后者包括阿尔茨海默病(AD)、帕金森病(PD)、亨廷顿病(HD)、肌萎缩性侧索硬化(ALS)。
炎症性肠病[IBD],包括克罗恩病[CD]和溃疡性结肠炎[UC],是一种在年轻时就会发病的炎症失调肠道疾病。虽然IBD的病因尚不清楚,但一个公认的假说是,微生物群、肠道上皮细胞和免疫细胞的某些成分一起导致了疾病的发生。全基因组关联研究发现,IBD患者有200多个基因位点,其中一些与其他疾病相关。最近,有报道称肠道炎症可能在帕金森病的发展中起作用。帕金森病是一种神经退行性疾病,以运动功能障碍为特征,例如运动迟缓、静止性震颤、身体僵硬和姿势不稳,以及非运动特征,如抑郁症、睡眠障碍和认知能力下降。
据估计,全球有1%的60岁以上人口受到影响。痴呆症是另一种缓慢进展的神经退行性疾病,其特点是逐渐的神经认知能力下降和慢性不可逆转的功能退化。阿尔茨海默病[AD]是最常见的痴呆病因,其特征是逐渐的神经认知衰退和长期的不可逆转的功能恶化。此外,全基因组关联研究显示,IBD和PD之间有相当多的遗传重叠。虽然以前的研究已经研究了IBD患者的PD风险增加,但很少有人研究IBD与PD的关系。本研究的目的调查在韩国全国范围内PD和AD的发病率以及与IBD的关系。
研究人员利用韩国国民健康保险服务对整个韩国人口的数据进行了分析,确定了 2009 年至 2011 年被诊断为 IBD 患者以及一部分合格的对照组,并对其进行了随访至 2017 年。根据年龄和性别以 1:4 的比例选择了对照组,以便与病例进行比较.
研究结果显示在 24830名IBD患者和99320名非IBD患者中,98 名 IBD 患者和 256 名对照发展为 PD,644 名 IBD 患者和 2303 名对照组患者发展为 AD。IBD 患者的总体神经退行性疾病风险较高(PD:[HR],1.56;95% [CI],1.24-1.97;AD:HR,1.14;95% CI,1.05-1.25)。与对照组相比,40-65 岁的年轻 IBD 患者发生 PD 的风险更高[HR,2.34;1.63-3.35]。相比之下,与对照组相比,年龄≥65 岁的患者患 AD 的风险增加 [HR,1.14;1.04-1.25]。在 IBD 队列的巢式病例对照研究中,年龄≥65 岁的患者和女性是 AD 的危险因素,而居住在城市地区则可以预防 AD的发生。
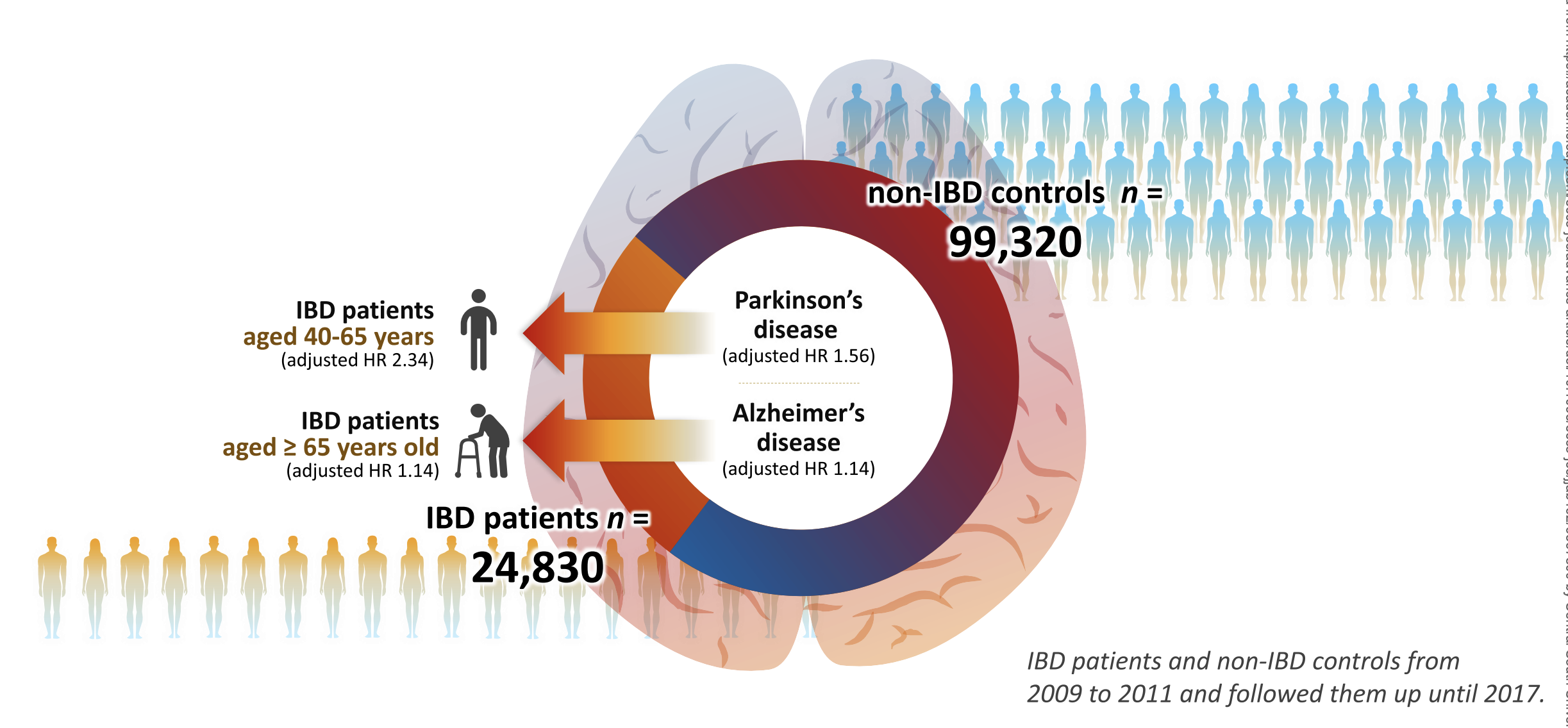
这项研究表明,韩国IBD患者的神经退行性疾病,如PD和AD的发病率高于韩国非IBD人群。年龄较大与神经退行性疾病的发展明显相关。然而,IBD患者发生早发性PD的风险增加。
原始出处:
Ga Hee Kim.et al. Risk of Neurodegenerative Diseases in Patients with Inflammatory Bowel Disease: A Nationwide Population-based Cohort Study.Journal of Crohn's and Colitis.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#退行性疾病#
81
#神经退行#
78
#疾病风险#
80
#炎症性#
51
#炎症性肠病患者#
83