JAMA:长检测间期ICD为临床适宜选择
2013-05-15 高晓方 译 医学论坛网
意大利一项研究表明,在接受置入型心律转复除颤器(ICD)治疗的患者中,长检测间期可实现抗心动过速起搏(ATP)和电击率降低,并可减少不适当电击。论文发表于《美国医学会杂志》。 此项随机单盲研究共纳入1902例置入ICD并且行一级和二级预防的缺血性和非缺血性病因患者。按1:1比率随机给予患者长检测间期(948例)或标准检测间期(954例)编程。主要转归为所有发作所传送的ATP和电击总数,次
意大利一项研究表明,在接受置入型心律转复除颤器(ICD)治疗的患者中,长检测间期可实现抗心动过速起搏(ATP)和电击率降低,并可减少不适当电击。论文发表于《美国医学会杂志》。
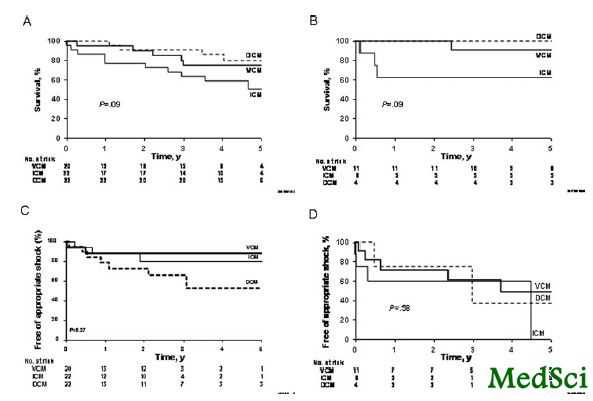
此项随机单盲研究共纳入1902例置入ICD并且行一级和二级预防的缺血性和非缺血性病因患者。按1:1比率随机给予患者长检测间期(948例)或标准检测间期(954例)编程。主要转归为所有发作所传送的ATP和电击总数,次要转归为不适当电击、死亡率和晕厥率。
结果显示,在中位12个月随访期间,长检测和标准检测间期组分别传送346次(42/100人年)和557次(67/100人年)治疗,ATP分别为23和37/100人年,电击分别为19和30/100人年。长检测间期组的总体治疗次数(ATP和电击)以及不适当电击均出现显著减少。两组患者在死亡率和心律失常晕厥率方面无显著差异。
与ICD相关的拓展阅读:
- Heartwire:ICD手术期间应用华法林或优于肝素过渡
- JCE:心肌淀粉样变性患者的ICD治疗
- Europace:ICD植入患者常合并睡眠呼吸障碍
- JAMA:ICD一级预防患者生存率在临床试验和临床实践中相似
- JCE:ICD可用于预防心脏病瓣膜病患者的心脏病猝死 更多信息请点击:有关ICD更多资讯

Effect of Long-Detection Interval vs Standard-Detection Interval for Implantable Cardioverter-Defibrillators on Antitachycardia Pacing and Shock DeliveryThe ADVANCE III Randomized Clinical Trial
Importance
Using more intervals to detect ventricular tachyarrhythmias has been associated with reducing unnecessary implantable cardioverter-defibrillator (ICD) therapies.
Objective
To determine whether using 30 of 40 intervals to detect ventricular arrhythmias (VT) (long detection) during spontaneous fast VT episodes reduces antitachycardia pacing (ATP) and shock delivery more than 18 of 24 intervals (standard detection).
Design, Setting, and Participants
Randomized, single-blind, parallel-group trial that enrolled 1902 primary and secondary prevention patients (mean [SD] age, 65 [11] years; 84% men; 75% primary prevention ICD) with ischemic and nonischemic etiology undergoing first ICD implant at 1 of 94 international centers (March 2008-December 2010).
Interventions
Patients were randomized 1:1 to programming with long- (n = 948) or standard-detection (n = 954) intervals.
Main Outcomes and Measures
Total number of ATPs and shocks delivered for all episodes (primary outcomes) and inappropriate shocks, mortality, and syncopal rate (secondary outcomes).
Results
During a median follow-up of 12 months (interquartile range, 11-13), long-detection group had 346 delivered therapies (42 therapies per 100 person-years, 95% CI, 38-47) vs 557 in the standard-detection group (67 therapies per 100 person-years [95% CI, 62-73]; incident rate ratio [IRR], 0.63 [95% CI, 0.51-0.78]; P < .001). The long- vs the standard-detection group experienced 23 ATPs per 100 person-years (95% CI, 20-27) vs 37 ATPs per 100 person-years (95% CI, 33-41; IRR, 0.58 [95% CI, 0.47-0.72]; P < .001); 19 shocks per 100 person-years (95% CI, 16-22) vs 30 shocks per 100 person-years (95% CI, 26-34; IRR, 0.77 [95% CI, 0.59-1.01]; P = .06), with a significant difference in the probability of therapy occurrence (P < .001); and a reduction in first occurrence of inappropriate shock (5.1 per 100 patient-years [95% CI, 3.7-6.9] vs 11.6 [95% CI, 9.4-14.1]; IRR, 0.55 [95% CI, 0.36-0.85]; P = .008). Mortality (5.5 [95% CI, 4.0-7.2] vs 6.3 [95% CI, 4.8-8.2] per 100 patient-years; HR, 0.87; P = .50) and arrhythmic syncope rates (3.1 [95% CI, 2.6-4.6] vs 1.9 [95% CI, 1.1-3.1] per 100 patient-years; IRR, 1.60 [95% CI, 0.76-3.41]; P = .22) did not differ significantly between groups.
Conclusions and Relevance
Among patients receiving an ICD, the use of a long- vs standard-detection interval resulted in a lower rate of ATP and shocks, and inappropriate shocks. This programming strategy may be an appropriate alternative.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ICD#
74