重磅:华人科学家发现阿尔茨海默病的源头或可追溯到出生前
2017-02-18 周伦 奇点
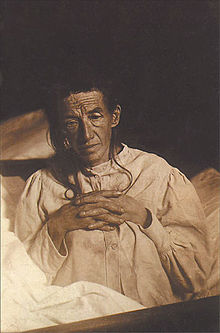
近期,来自加拿大不列颠哥伦比亚大学(University of British Columbia)的宋伟宏教授团队和重庆医科大学附属儿童医院的李廷玉教授团队,在阿尔茨海默病开始的时间这个问题上,有了最新的惊人发现:如果胎儿或新生儿没有获得足够的维生素A,导致阿尔茨海默病的生物化学反应可能在婴儿还在子宫内或刚出生后就开始了。他们的这一重要研究成果刊登在神经学领域的著名期刊《Acta Neuropat
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿尔茨#
60
#科学家发现#
79
#阿尔茨海#
72
#阿尔茨海默#
55
#重磅#
71
#华人#
74