Chin Med J :韩雅玲院士团队发现:通心络可减少冠脉介入术后患者血小板高反应性
2018-03-09 朱柳媛 中国循环杂志 发表于威斯康星
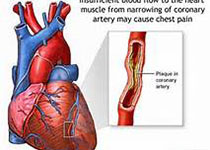
对于接受经皮冠脉介入治疗的急性冠脉综合征患者来说,术后氯吡格雷治疗期间如果出现血小板高反应性,意味着发生缺血事件的风险较高。
近期,沈阳军区总医院韩雅玲院士研究团队公开的一项前瞻性、多中心、随机、双盲、安慰剂对照研究提示,通心络胶囊有降低血小板高反应性和高敏C反应蛋白水平的作用。
因此,研究者认为,冠脉介入治疗术后阿司匹林和氯吡格雷双联抗血小板治疗时出现血小板高反应性的急性冠脉综合征患者,可考虑联合通心络治疗。
这项研究纳入136例冠脉介入治疗术后存在血小板高反应性的急性冠脉综合征患者,在标准双联抗血小板治疗的基础上,随机给予安慰剂或通心络胶囊治疗。
治疗30天时,两组中有血小板高反应性的患者比例均显着降低,但通心络胶囊组降幅显着大于安慰剂组(24.8% vs 15.8%, P=0.013),这在携带1个细胞色素P450 2C19功能缺失等位基因的患者中更明显。通心络胶囊组的血小板高反应性比例也明显低于安慰剂组(33.3% vs 54.2%),但两组的缺血事件发生率并无显着差异。
原始出处:
Zhang L, Li Y, Yang BS, et al. A Multicenter, Randomized, Double-Blind, and Placebo-Controlled Study of the Effects of Tongxinluo Capsules in Acute Coronary Syndrome Patients with High On-Treatment Platelet Reactivity. Chin Med J (Engl). 2018 Mar 5;131(5):508-515.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血小板高反应性#
73
#韩雅玲院士#
76
#反应性#
95
#韩雅玲#
86
#冠脉介入术#
79
#Med#
56
学习了受益匪浅
101