Human Gene Therapy:非病毒基因载体技术治疗B细胞淋巴瘤研究进展
2016-12-27 生物帮 生物帮
近日,国际知名杂志《Human Gene Therapy》上发表在线了中国科学院深圳先进技术研究院陈志英研究团队题为“Treatment of human B-cell lymphomas using minicircle DNA vector expressing anti-CD3/CD20 in a mouse model”的研究文章。论文报道该团队的核心技术非病毒基因载体微环DNA表达双
近日,国际知名杂志《Human Gene Therapy》上发表在线了中国科学院深圳先进技术研究院陈志英研究团队题为“Treatment of human B-cell lymphomas using minicircle DNA vector expressing anti-CD3/CD20 in a mouse model”的研究文章。论文报道该团队的核心技术非病毒基因载体微环DNA表达双靶向抗体治疗人B细胞淋巴瘤。
近年来,癌症免疫治疗有重大突破,若干治疗技术使部分病人病情长期稳定甚至痊愈,表明免疫治疗是人类攻克癌症的希望所在。微环DNA表达双靶向抗体的癌症免疫治疗技术成为继CAR-T技术(“嵌合抗原受体T细胞免疫疗法”)、TIL技术(“肿瘤渗润淋巴细胞技术)、免疫检查点抑制剂等技术之后又一项获得成功的新一代治疗技术。
陈志英团队多年来致力于研究微环DNA表达双靶向抗体的癌症免疫治疗技术。微环DNA是陈志英团队发明的一种非病毒基因载体,因其卓越的基因表达功能,方便的制备技术,已被全球生物医学界广为应用,并在全世界销售。双靶向抗体是一种成熟的抗癌技术,通过链接病人体内的T细胞和癌细胞,达到杀灭癌细胞的目的,其应用比CAR-T和TIL技术方便,FDA已经批准两种双靶向抗体进入市场。但提纯的双靶向抗体半衰期短,需要用微泵连续给药,非常不便,费用高昂。
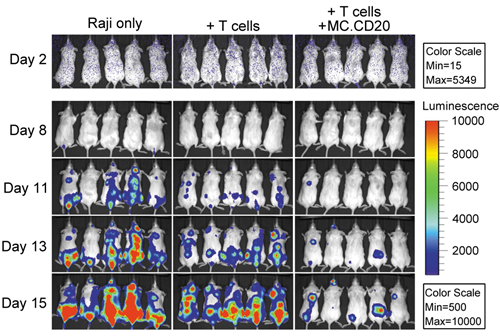
最近,陈志英团队取得相关进展,是用带有萤火虫荧光基因的人B细胞淋巴瘤细胞株Raji接种到免疫缺陷小鼠,然后将微环DNA(MC.CD20)一次注射到小鼠肝脏,在体内持续表达治疗水平的抗B细胞淋巴瘤(抗-CD3/CD20)的双靶向抗体,并提供人的T细胞。因为Raji细胞在小鼠发出的荧光与癌细胞成正比,用小动物成像仪可以实时监测疗效(如图)。结果标明,同时接受MC.CD20与人T细胞的治疗组小鼠瘤负荷显着低于对照组,生命显着延长,证明抗癌微环DNA治疗癌症的可行性。目前,陈志英团队正在开发把微环DNA注射到肌肉表达抗癌双靶向抗体的技术,一旦成功,便可实现“治疗癌症如打疫苗”一样安全、方便、可负担。微环DNA在肌肉表达抗癌双靶向抗体技术可能为人类攻克癌症做出重要贡献。
 载体技术治疗B细胞淋巴瘤研究进展">
载体技术治疗B细胞淋巴瘤研究进展">B细胞淋巴瘤Raji细胞携带荧光基因,图中治疗组(T Cells+MC.CD20)小鼠荧光强度显着少于对照组(Raji only和T cells),表明微环DNA表达抗-CD3/CD20抗体大大降低瘤负荷,有显着疗效
原始出处:
Treatment of human B-cell lymphomas using minicircle DNA vector expressing anti-CD3/CD20 in a mouse model.Human Gene Therapy
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ERA#
43
#非病毒#
63
#载体#
62
#Gene#
60
#细胞淋巴瘤#
52
#human#
48
#B细胞#
53
#研究进展#
51