一周研究进展荟萃:让你知识满满!
2015-09-08 MedSci MedSci原创
通宵工作 癌细胞 β受体阻滞剂 睡眠 阿片类药物 心衰 动脉硬化

1. NEJM:通宵值班后,次日手术,外科医生还扛得住么?
发表于《新英格兰杂志》的新研究,对外科医生在手术当天的前一晚通宵工作后,是否会导致患者不良预后风险的增加进行了探讨。
之前的研究表明,急性睡眠剥夺可影响人的情绪,并损害认知功能,但是其对医生临床技能造成多大的影响,仍不得而知。
研究人员将38978例患者平均分为了两组:在1组中,医生在手术前一天通宵工作(午夜至第二天7点);另一组,医生未通宵工作。
结果显示,手术前一天晚上通宵工作,并没有对第二天的手术造成显著影响;仅发现,在手术前一晚曾进行过2-3项手术的医生,第二天进行手术时手术的并发症才会有轻微的增加。
最后,研究人员对这一结果与之前针对实习医生进行的研究结果的不同进行了猜测:除了有更多的经验外,主治医生在感觉疲劳不能进行手术的情况下,可通过取消手术或安排其他同事替他们进行手术,此外,预期经过一夜的待命,第二天会出现睡眠剥夺时,医生可能会调整他们的工作量。
2. NCB:癌变的细胞能恢复正常?!
科学家们一直有一个梦想,希望有一天能够将肿瘤细胞再变回正常细胞。最近,科学家们在追逐梦想的路上完成了一次飞跃。
过往的研究发现E-cadherin和p120 catenin这两个黏附蛋白具有两面性:一方面维持正常的组织形成,另一方面能够促进肿瘤发生。但它们究竟如何受到调控并在促癌和抑癌之间发生转换仍未可知。
在最新的研究中发现一种名叫PLEKHA7的蛋白能够与E-cadherin和p120 发生相互作用,能够将一组前体miRNA招募到E-cadherin和p120定位的顶端粘着小带,并将其加工为一组特定的miRNA,进而调控一些与细胞转化有关的基因表达以维持细胞正常形态。但在正常极化的上皮细胞中,这种相互作用只会发生在细胞顶部。而在癌细胞中PLEKHA7发生缺失则会导致这组miRNA失调,导致E-cadherin和p120促进肿瘤生长。在实验条件下恢复癌细胞中正常的miRNA表达水平可以逆转癌细胞的异常生长。
这项研究第一次将细胞黏附与miRNA生物学两个不同的研究领域联系在一起,并解释了一个长久以来一直存在争议的问题,同时也为癌症治疗策略的开发提供了重要信息。
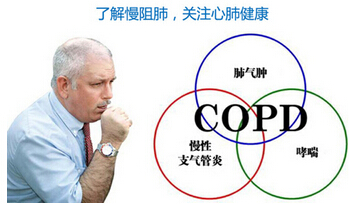
3.BMJ:β受体阻滞剂可减少COPD的急性发作
背景:一些回顾性研究已经表明,在COPD患者身上使用β阻滞剂可降低急性发作率与死亡率。但也有人担心这对于使用家庭氧疗的严重的COPD患者可能是有害的。
方法:以全球倡议COPD黄金阶段2-4分期为主题参与COPDGene的前瞻性随访列队研究。在调整人口结构。气流阻塞,CT表明肺气肿百分率,呼吸系统药物,冠状动脉疾病,充血性心力衰竭和冠状动脉钙化后作出使用β阻滞剂的倾向,并使用负二项回归分析比较了组间分类β阻滞剂纵向使用后的总的严重恶化率。
结论:无论气流阻塞的严重程度,β阻滞剂的使用都显著降低慢性阻塞性肺疾病的急性加重发生率。
研究发现,β受体阻滞剂在严重的COPD中可显著减少急性发作,在潜在的心血管疾病及其倾向药物的调整后依然奏效。还发现,使用其他心脏药物如CCBs和ACEI/ARB并没有降低急性加重的风险,这表明β阻滞剂有显著作用。

4.Sleep:睡眠不足,更易感冒?
研究人员认为:相比人们的年龄、压力水平、种族、受教育水平、收入、是否吸烟等因素,睡眠时间短相比其他任何因素更易导致民众感冒。
既往研究认为,睡眠不足可能会影响机体健康,并会增加心脏病发作和中风的风险。但是美国民众普遍不能获得足够睡眠。根据国家睡眠基金会,1/5的美国人每个工作日的睡眠时长不足6个小时。
研究人员选取了164名受试者,对他们进行长达2个月的体检,同时也监测他们的睡眠状况。之后通过鼻腔给予他们感冒病毒,研究人员分析了机体对病毒的抵御能力。
结果发现:每日睡眠不足6个小时的受试者患感冒的几率是比睡眠时长超过7个小时的人的4.2倍。睡眠时长不到5个小时的参与者感冒风险更高,是睡眠时长超过7个小时的民众的4.5倍。
虽然这项研究进一步验证了睡眠对维持民众身体健康的重要性,但是研究人员认为,还需要更进一步的研究扭转人们对睡眠的态度,正视睡眠问题并改善睡眠状况。

5.JAMA Intern Med:防止阿片类药物滥用的新策略
美国佛罗里达州一直致力于减少处方阿片类药物的滥用和处方分配问题,一项最新研究显示,通过处方药物管理办法(PDMPs)和“药物滥用”法使得阿片类药物处方的开具和使用有了一定的缓解。
阿片药物使用、上瘾和过量引起的死亡从20世纪中期开始泉涌出现,而佛罗里达州正是这个问题的核心地区。佛罗里达州立法机关通过了一个法案,该法案要求诊所在州里进行登记并且必须有一个内科医师,而且需要建立严格的开具处方和分发药物的规定。2011年,该州的PDMP开始实施。
最后,研究人员评论道“我们的结果关键是考虑到了阿片药物处方滥用的上升趋势,同样也说明了州政府在为了抵制这种趋势所立的法案中扮演了一个重要角色”。

6.JACC:心衰患者心脏康复治疗,你知道多少?
背景:目前指南推荐病情稳定的门诊心脏衰竭(HF)患者进行心脏康复训练(CR);然而,现实是心衰患者与心脏康复治疗相关的治疗趋势及其影响因素并不完全已知。
目的:旨在评估失代偿心衰出院患者心脏康复的使用率,趋势以及影响因素。
方法:数据来自国家心衰指南,研究评估了2005年至2014年间,射血分数降低型心衰(HFrEF)和射血分数保留型心衰(HFpEF)患者出院后,其心脏康复训练的趋势。同时,研究通过多变量分析评估了患者、医院等级与心脏康复训练之间的联系。
结论:只有10%的心衰患者出院后愿意接受心脏康复治疗。其接受程度随着HFrEF和HFpEF患病时间的延长而增加。应该使用额外的治疗策略提高心衰患者和医生对于心脏康复治疗获益的意识。

7.Stroke:高水平IL-16可降低人类动脉粥样硬化的风险
白细胞介素16(IL-16)是T细胞生长的调节因子,是细胞迁移的诱导剂。本研究的目的是要确定的IL-16在人的颈动脉斑块中的测定是否与症状(例如卒中、短暂性脑缺血发作、或一过性黑蒙),斑块稳定性标志物和手术后的心血管事件相关联。
研究人员对动脉内膜切除术前1个月内发生≥1脑血管缺血性事件中获得斑块(n=111)与无症状患者的斑块(n=95)进行了比较。对中性脂质、平滑肌细胞和巨噬细胞含量通过组织学评价,胶原蛋白、弹性蛋白和Caspase-3活性通过生物化学反应进行了测定。IL-16、CD3、CD4、和FoxP3的mRNA在颈动脉斑块中的表达通过实时定量聚合酶链反应进行了分析。
研究表明,高水平的IL-16与无症状颈动脉斑块,因素促成斑块的稳定性表达,以及手术后2年期间新的心血管事件的危险性下降相关。这表明IL-16可能在人类动脉粥样硬化中有一定的保护作用。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









谢谢分享。
193
了解
150
#荟萃#
68
#研究进展#
71
一大早读一读,收获满满
202
生活质量好才是好
142