JCO:围手术期肝动脉灌注化疗可延长结直肠癌肝转移切除术后生存:一项倾向评分分析
2017-07-05 JCO肿瘤论坛 JCO肿瘤论坛
Bas Groot Koerkamp, Eran Sadot, Nancy E. Kemeny, Mithat Gonen, Julie N. Leal, Peter J. Allen, Andrea Cercek, Ronald P. De Matteo, T. Peter Kingham, William R. Jarnagin, and MichaelI. D’Angelica本刊负责人
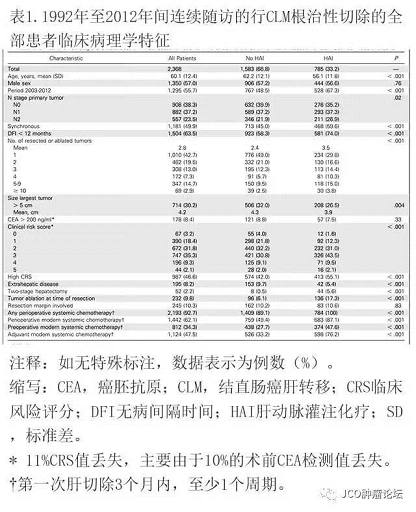
目的:本项研究试图分析围手术期肝动脉灌注化疗(HAI)是否与结直肠癌肝转移(CLM)完全切除患者的总生存期(OS)相关。方法:统计来自单中心数据库1992年至2012年间CLM完全切除的患者。所有接受HAI的患者同时也接受过围手术期全身化疗。应用倾向评分分析按照七项已知的预后因素匹配患者。结果:共有2,368例接受CLM完全切除患者入选,中位随访时间为55个月。尽管HAI组中晚期病例更多,但其中位OS(n = 785)为67个月,未接受HAI组为44个月(n = 1,583; P<0.001)。HAI组10年生存率为38.0%,未接受HAI组为23.8%。对于接受现代全身化疗(n = 1,442)的患者,HAI组中位OS为67个月,未接受HAI组为47个月(P< 0.001)。倾向评分调整风险比表明HAI组有较长的OS:0.67(95%CI,0.59?0.76; P< 0.001)。针对淋巴结转移阴性(HAI组为129个月v未接受HAI组为 51个月; P< 0.001)及临床风险评分低至0至2分(HAI组为89个月v未接受HAI组为月为53个月; P<
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#手术期#
64
#切除术#
50
#JCO#
48
#肝转移#
66
#结直肠#
64
竟然全文翻译了!学习了
85
继续学习。
83