Neurology:10年前瞻性队列研究,慢性肾脏疾病与短暂性脑缺血发作/脑卒中前后痴呆发生无独立相关!
2022-02-04 Naomi MedSci原创
近日有研究人员试图确定在短暂性脑缺血或卒中前后 CKD 和所有原因的痴呆症之间的联系,研究表明CKD 与脑血管事件发生前后痴呆均无独立关系,这表明肾脏特异性机制不太可能在病因学中发挥重要作用。
慢性肾脏病(CKD)伴随着严重的认知功能损害和肾功能的下降。在卒中的地域和种族差异的研究中,EGFR< 60ml/min/1.73 m2时,每下降10ml/min/1.73 m2与认知功能障碍患病率增加11% 相关。血液透析患者有严重认知功能损害的可能性是年龄匹配的非透析患者的3倍,其患病率达30-40% 。
此外,慢性肾脏病患者的执行功能和处理速度明显受损,这与脑血管疾病一致。虽然慢性肾脏病也可能随着高血压和阿尔茨海默病的病理学相互作用而增加,或通过神经毒素如神经兴奋剂胍化合物的高浓度而增加,慢性肾脏病和神经退行性疾病痴呆之间的任何联系可能仅仅是由于慢性肾脏病患者的脑血管疾病增加。然而,在以前的一项研究中,CKD预测了所有原因的痴呆,而不是先前的症状性脑血管疾病和脑部小血管疾病。为了探讨血管假说,近日有研究人员试图确定在短暂性脑缺血或卒中前后 CKD 和所有原因的痴呆症之间的联系。
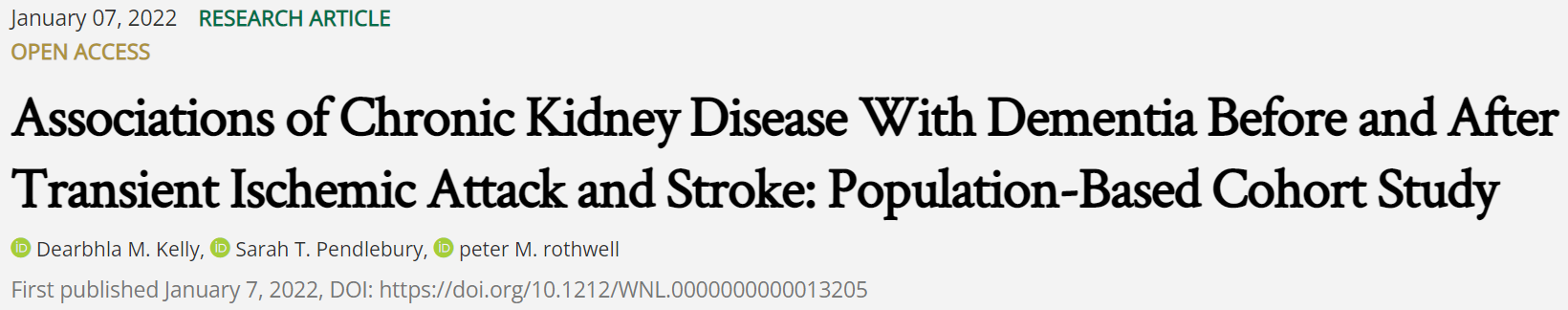
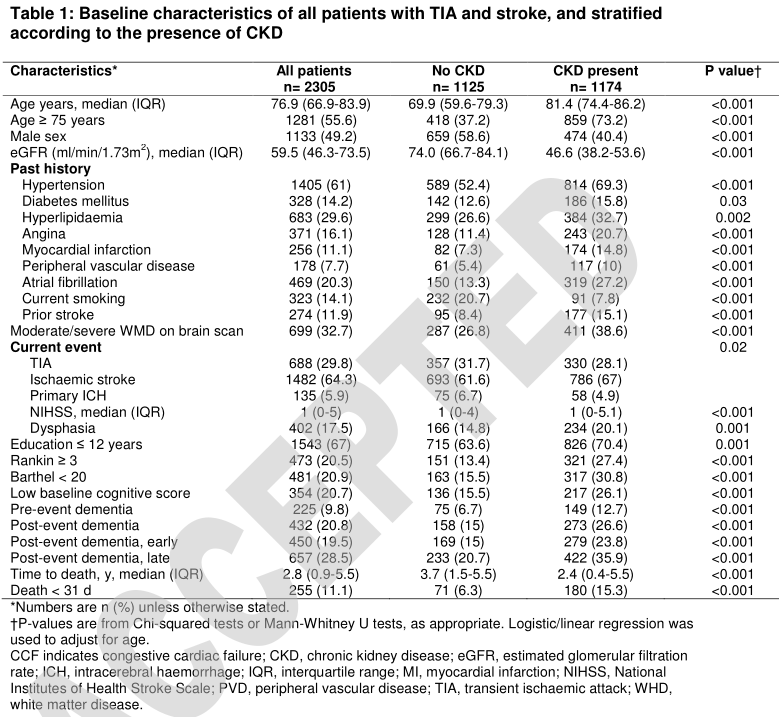
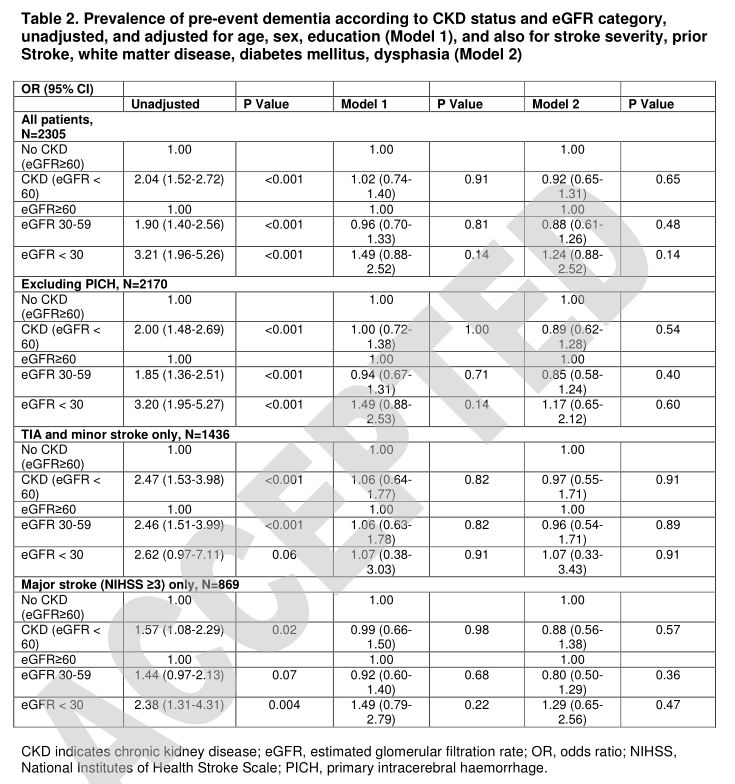
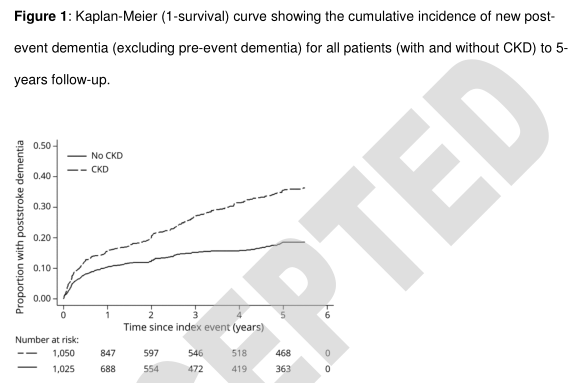
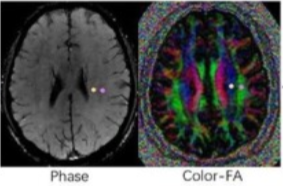
在一项以人群为基础的短暂性脑缺血和卒中前瞻性队列研究(牛津大学血管研究; 2002-2012年)中,通过对患者的直接评估和5年的随访,以及对医院/基层医疗记录的审查,确定事前和事后痴呆症。研究人员使用肾功能 Logit模型检测事件前痴呆和 CKD (定义为估计的[EGFR] < 60ml/min/1.73 m 2)之间的关系,并使用COX和竞争风险回归模型检测事件后痴呆和 CKD 之间的关系,根据年龄、性别、教育程度、卒中严重程度、卒中前期、白质疾病、糖尿病和言语困难进行调整。
- 2305例TIA /卒中患者被纳入(中位年龄77岁[67-84岁] ,男性1133例[49% ] ,TIA 688例[30% ]),其中CKD 1174例(50.9%)。
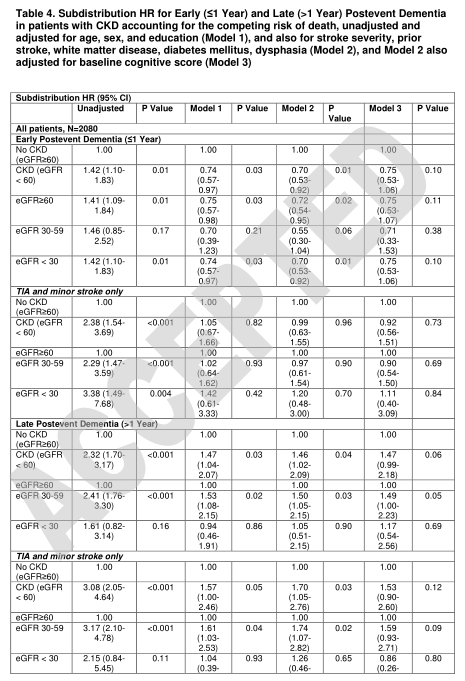
- CKD 与脑血管事件发生前(优势比[ or ] ,2.04[95% CI,1.52-2.72] ; p < 0.001)和脑血管事件发生后痴呆(危险比[ hr ] ,2.01[95% CI,1.65-2.44] ; p < 0.001)均有关联,但这些关联在协变量调整后减弱(或 = 0.92[0.65-1.31] ; p = 0.65和 = 1.09[0.85-1.39] ; p = 0.50)。
- 采用竞争风险模型时,结果相似(子分布 hr [ shr ] = 1.74[1.43-2.12; p < 0.001,经调整后衰减至1.01[0.78-1.33] ; p = 0.92)。
- CKD 与脑血管事件发生晚期(> 1年)痴呆(shr = 2.32,1.703.17; p < 0.001)相关性较强,尤其是TIA和轻度脑卒中(shr = 3.08,2.05-4.64; p < 0.001) ,但调整后无显著性差异(shr = 1.53,0.90-2.60; p = 0.12)。
在短暂性脑缺血发作和脑卒中患者中,CKD 与脑血管事件发生前后痴呆均无独立关系,这表明肾脏特异性机制不太可能在病因学中发挥重要作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Neurol#
80
#前瞻性队列研究#
85
#短暂性脑缺#
100
#前瞻性#
69
#前瞻性队列#
96
#短暂性#
86
非常有用
112
#脑缺血#
107
#慢性肾脏#
112
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
0