Circulation:IDO,急性心肌梗死治疗的新靶点!
2021-02-14 MedSci原创 MedSci原创
吲哚胺2,3 -双加氧酶1 (IDO)催化L-色氨酸代谢的一个限速步骤,还是多种病理条件的重要调节因子。
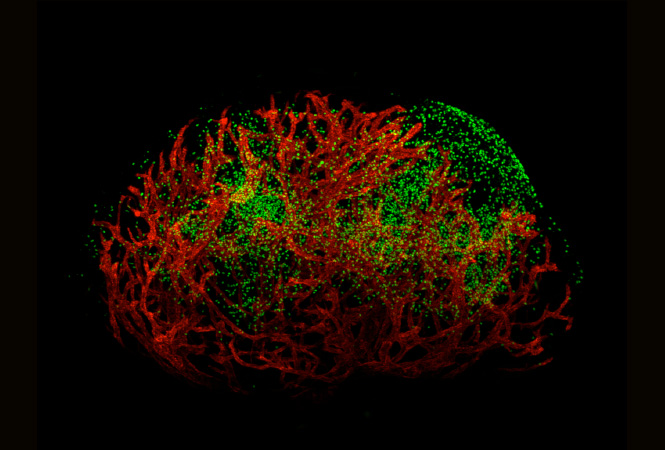
缺血性心血管疾病,特别是急性心肌梗死(MI),是世界范围内主要的死亡原因之一。吲哚胺2,3 -双加氧酶1 (IDO)催化L-色氨酸代谢的一个限速步骤,还是多种病理条件的重要调节因子。Melhem等人推测IDO可能在MI后心脏稳态的局部调节中起关键作用。
本研究分析了具有不同特异性细胞IDO缺陷的小鼠的心肌修复(特异性细胞包括:内皮细胞、平滑肌细胞、心肌细胞、髓细胞,以及急性心肌梗死时的心肌修复。
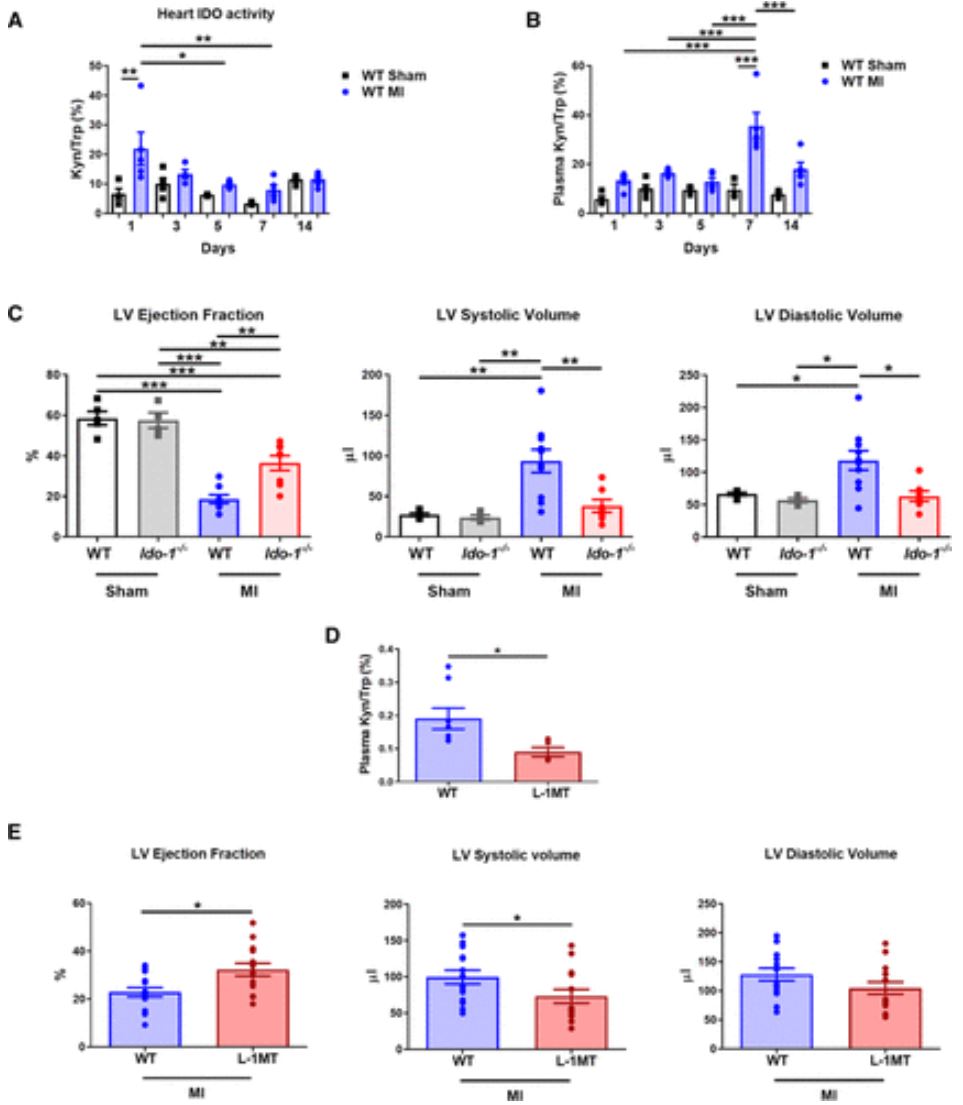
IDO缺陷/抑制可限制MI后的心脏功能障碍
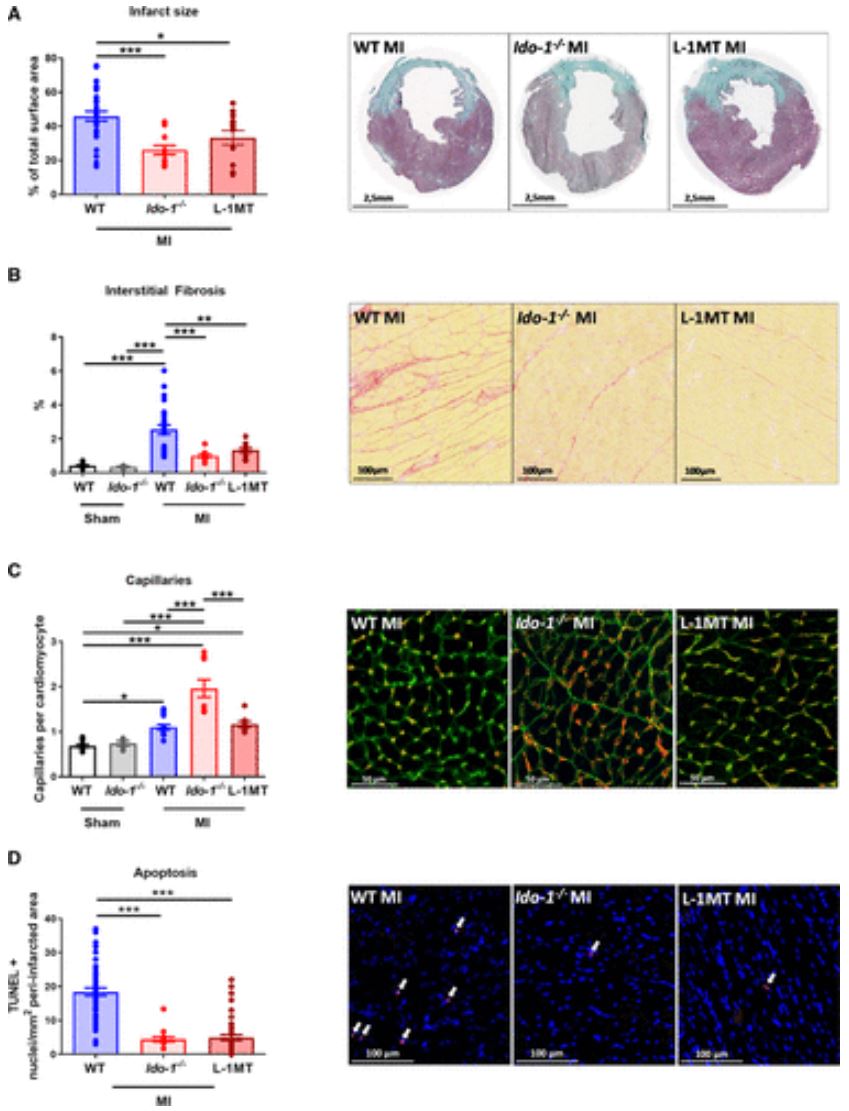
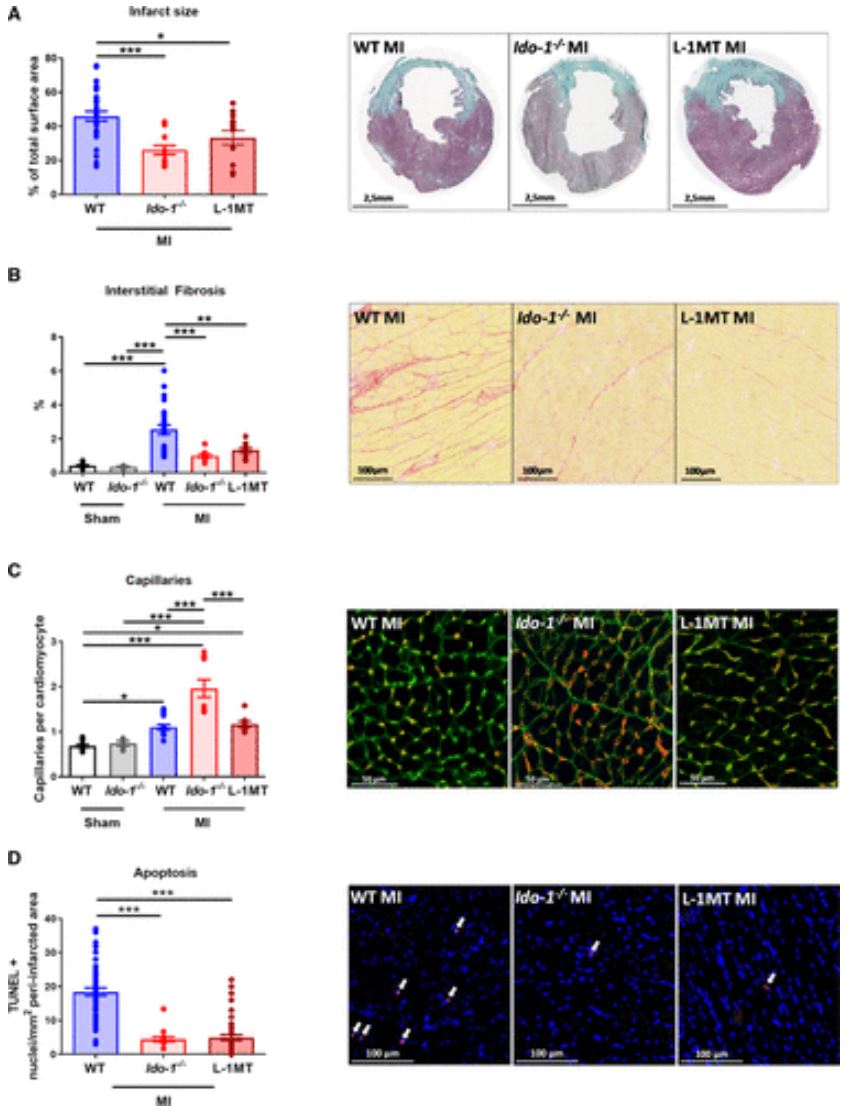
研究结果显示,小鼠MI后通过IDO产生的肾素受到明显诱导。敲除或药理抑制IDO会限制MI后的心脏损伤和心功能障碍。平滑肌细胞、炎症细胞或心肌细胞的IDO功能明显丧失并不影响小鼠MI后的心脏功能和心室重构。
IDO缺陷/抑制可改善MI后心肌恢复
与此明显不同的是,内皮细胞特异性缺失IDO的小鼠的心脏功能和心肌细胞收缩能力均有所改善,而且不良心室重构也有所减弱。给IDO缺陷的小鼠补充犬尿氨酸可减弱IDO敲除的保护作用。犬尿氨酸通过一种芳基烃受体依赖性的机制产生活性氧来促进心肌细胞凋亡。
本研究数据表明,IDO可成为急性心肌梗死治疗的新靶点。
原始出处:
Nada Joe Melhem, et al. Endothelial Cell Indoleamine 2, 3-Dioxygenase 1 Alters Cardiac Function After Myocardial Infarction Through Kynurenine. Circulation. 2021;143:566–580
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#IDO#
115
#Circulation# 插入话题+积分
126
#新靶点#
90
i do
113
认真学习了
137