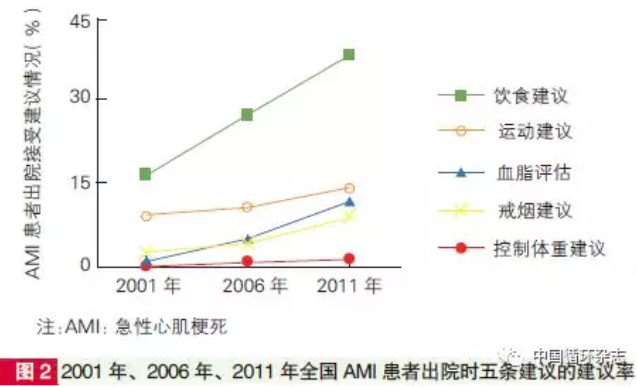
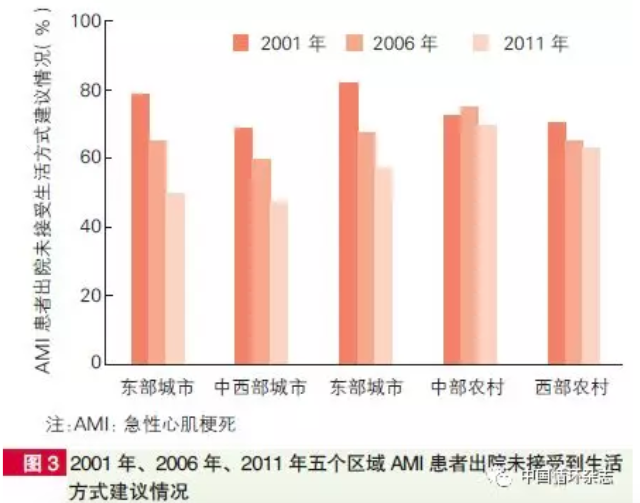
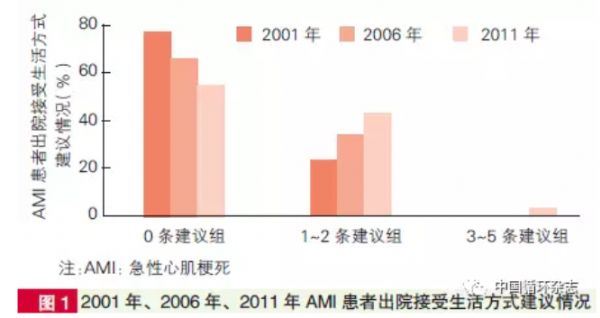
中国循环杂志:China Peace亚组研究:中国心梗患者改善生活方式建议严重不足
2018-02-12 卢芳 中国循环杂志
有研究显示,有效的健康宣教和干预,在降低急性心梗死亡率中会起到44%的作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CHINA#
90
#心梗患者#
69
#PE#
63
#ACE#
0
学习了.获益匪浅
104
学习了.获益匪浅!感谢分享
89