AGA指南在胰腺囊肿检出进展期肿瘤方面准确性欠佳
2016-06-16 高晓方 译 中国医学论坛报
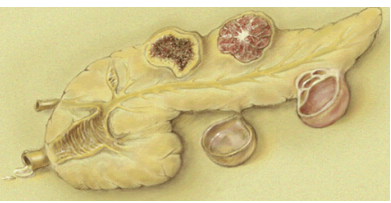
美国一项研究表明,美国胃肠病学会(AGA)指南在胰腺囊肿检出进展期肿瘤方面的准确性欠佳,综合分子检测的替代方法更具应用前景,但仍需进一步验证。论文发表于《消化内镜》杂志6月刊[Gastrointest Endosc2016,83(6):1107]。 该研究纳入225例因胰腺囊肿接受超声内镜引导下细针穿刺抽吸(EUS-FNA)检查的患者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好
85
#准确性#
61
#进展期#
72
#AGA#
0
好文章,值得学习
115
#囊肿#
48
#胰腺囊肿#
66