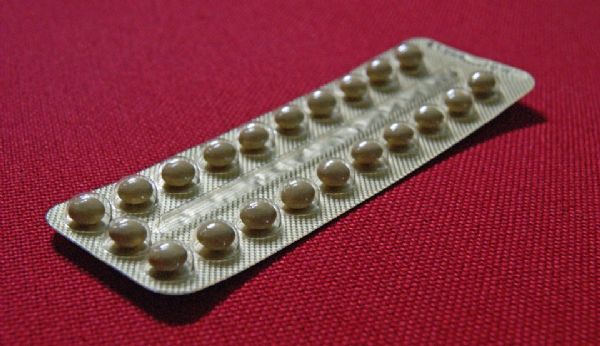
盘点:细数“避孕药”的功与过!
2016-09-08 MedSci MedSci原创
口服避孕药,通常被称为避孕药,是一种激素避孕药,美国每年大约有1200万名妇女采用口服避孕药的方式避孕。避孕药是一种非常有效的避孕方法。每年约8%的女性因忘记服用避孕药而发生意外怀孕。然而,若每天同一时刻服用避孕药,100位女性中只有一位会在使用避孕药的第一年内意外怀孕。除了能避孕,还存在以下几大好处: 1,10年调查发现,口服避孕药可降低癌症死亡率近日,发表在《Annals of
本文系梅斯医学(MedSci)原创编译整理,欢迎转载!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













了解以前没有认识的领域知识,赞一个。
100
很好的文章,学习学习
91
阅读了谢谢。
100
谢谢分享!
99
继续关注!
135
学习啦,,,
93
谢谢分享,,
97
很不错的文章
52