Signal Transduct Target Ther:人脐带血间充质干细胞治疗银屑病
2022-08-15 医路坦克 MedSci原创
银屑病是一种常见的慢性免疫介导的全身性疾病,本文评估了UMSC输注治疗银屑病的安全性和有效性。我们分析了免疫细胞亚群和血清细胞因子的变化,以探讨UMSCs可能的作用机制。
银屑病是一种常见的慢性免疫介导的全身性疾病,由多基因遗传决定,由多种环境因素诱发。银屑病的患病率在世界人口中从0.27%到11.43%不等。银屑病是一种先天和获得性免疫系统紊乱的疾病,树突状细胞、中性粒细胞、角质形成细胞和T细胞在发病机制中发挥主要作用。
当遗传易感个体暴露在感染、应激或创伤中时,皮肤树突状细胞被激活,产生肿瘤坏死因子α和白介素23,从而刺激促炎T细胞的增殖和分化。促炎症T细胞分泌炎症细胞因子,包括干扰素-γ和IL-17,它们作用于角质形成细胞和其他白细胞,形成放大的免疫应答。免疫学和遗传学研究证实IL-17/IL-23轴是银屑病发病的关键驱动因素。
间充质干细胞是一种多能细胞,具有再生能力和免疫调节特性。MSCs在体外对T细胞、B细胞和其他天然免疫细胞具有免疫调节功能,主要是通过细胞间接触或旁分泌机制,分泌细胞外小泡和细胞因子,包括转化生长因子-β(转化生长因子-β)、一氧化氮(NO)、吲哚-吡咯-2,3-双加氧酶(IDO)、肿瘤坏死因子刺激基因-6(TsG-6)、前列腺素E_2(PGE_2)和IL-10.骨髓间充质干细胞可减少引流淋巴结(DLN)中Th1细胞的数量,增加Tregs的数量,增加脾中Th2细胞的百分比,降低Th17细胞的频率,并增加关节和唾液腺中IL-10的水平。皮下注射间充质干细胞可显著降低皮损中产生IL-17的γδT细胞的百分比,降低皮损中IL-17的水平。我们先前的研究表明,静脉注射骨髓间充质干细胞还可以通过调节脾和外周血中Th1、Th2和Th17的平衡,抑制中性粒细胞的功能,下调浆细胞样树突状细胞产生干扰素-α,从而显著减轻银屑病模型小鼠的病情严重程度、皮肤炎性细胞浸润和血清细胞因子的产生。
在这项研究中,我们进行了1/2a期研究,以评估UMSC输注治疗银屑病的安全性和有效性。我们分析了免疫细胞亚群和血清细胞因子的变化,以探讨UMSCs可能的作用机制。
17例银屑病患者接受了UMSC输注。分析不良事件、实验室参数、PASI和PGA。治疗过程中及6个月随访未见明显不良反应。根据PGA评分,47.1%(8/17)的银屑病患者的PASI评分至少有40%的改善,17.6%(3/17)的患者没有疾病迹象或病情轻微。有效率男性为25%(2/8),女性为66.7%(6/9)。银屑病患者经UMSCT治疗后,外周血中Tregs和CD4+记忆性T细胞频率显著升高,辅助性T细胞(Th)17和CD4+初始T细胞频率显著下降。所有应答者在UMSCT后Tregs和CD4+记忆性T细胞显著增加,Th17细胞和血清IL-17水平显著降低。应答者的基线Tregs水平显著低于无应答者。
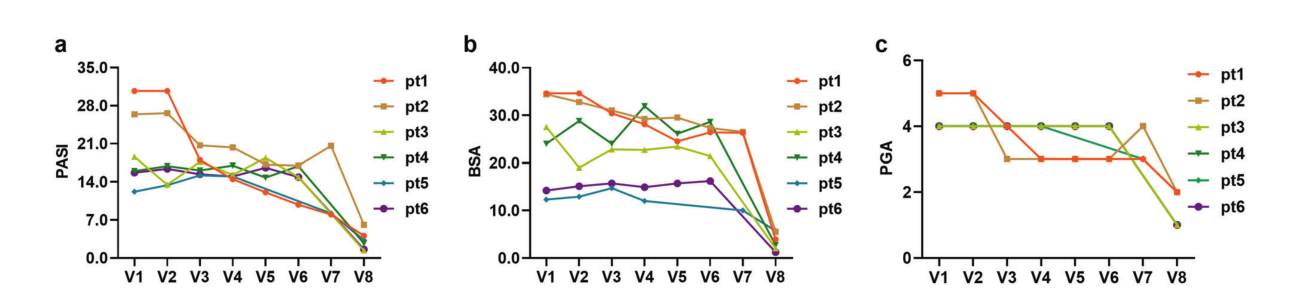
图中显示了6名应答者的三项结果指标,包括PASI评分、BSA和PGA。A PASI评分;b BSA;c PGA
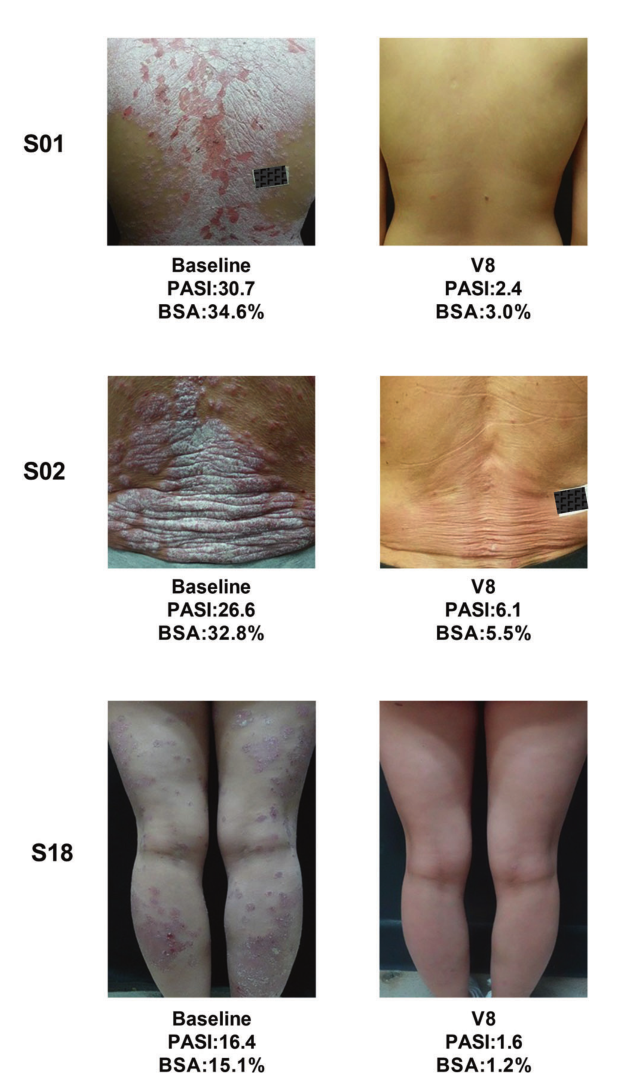
3例患者治疗前后的典型皮肤影像
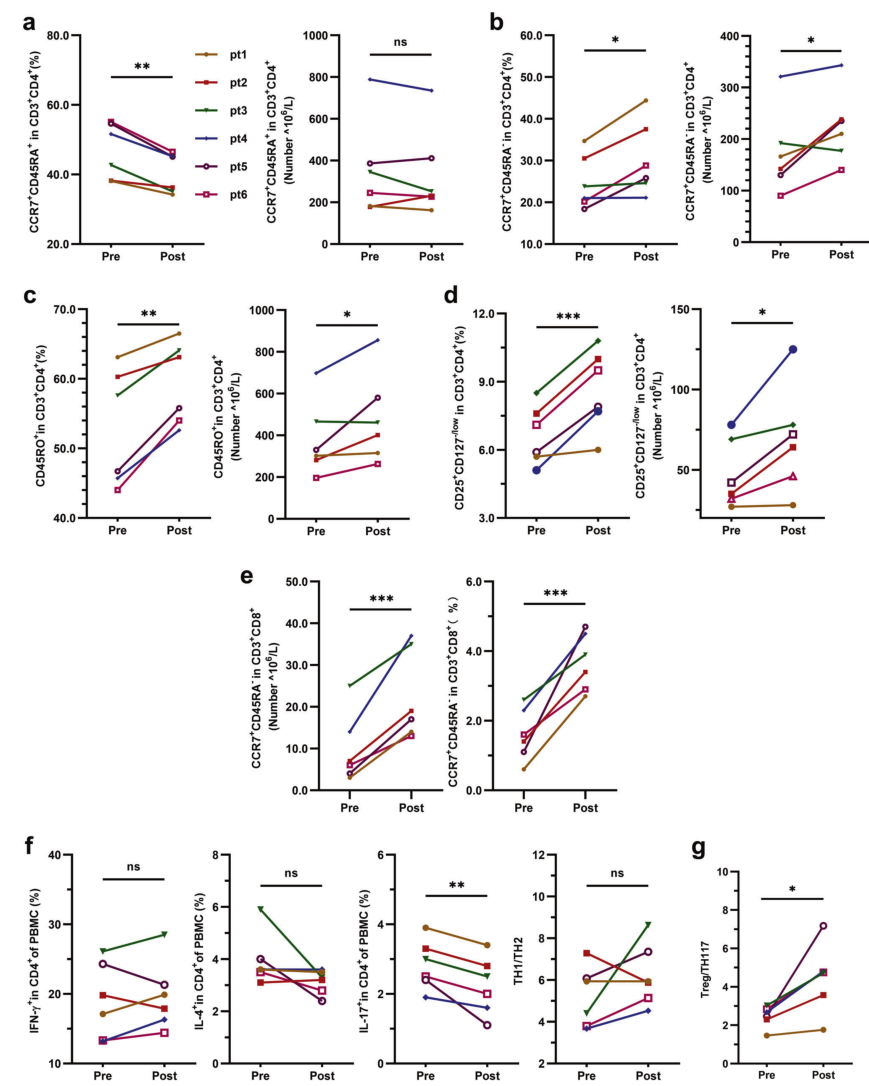
UMSCT前后应答者T淋巴细胞亚群的变化。应答者外周血中CD_4初始T细胞、CD_4+Tcm细胞、CD_4+记忆性T细胞、T细胞亚群和CD_8~+T细胞的频率和数量的变化(n=6,*P<0.001,**P<0.01,*P<0.001),外周血中Th1、T_2、T_1/T_2和T_1/T_2的频率和T细胞亚群的变化(n=6,*P<0.001,**P<0.01)
结论:同种异体UMSCT治疗银屑病安全、部分有效,Tregs水平可作为预测UMSCT临床疗效的有效生物标志物。
文献来源:Cheng L, Wang S, Peng C, Human umbilical cord mesenchymal stem cells for psoriasis: a phase 1/2a, single-arm study.Signal Transduct Target Ther 2022 Aug 05;7(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TRA#
87
#target#
88
#Signal#
97
#间充质干细#
87
#Sign#
87
#脐带血#
102
#脐带#
102