快速上手指南:原发性腹膜后软组织肿瘤的诊疗
2016-08-16 张波 肿瘤时间
软组织肿瘤主要是指一大类源于间叶组织的肿瘤,传统上还包括了周围神经源性的肿瘤,胚胎发生上主要源于中胚层和神经外胚层。腹膜后腔是指位于横膈以下盆膈以上,后壁层腹膜与腹横筋膜间的潜在腔隙,是软组织肿瘤的好发部位之一。原发性腹膜后肿瘤是指源于腹膜后腔非特定脏器的一大类肿瘤,其中逾半数以上为软组织肉瘤。原发性腹膜后软组织肿瘤(后简称「腹膜后肿瘤」)涵盖了数十种组织学类型和生物学行为方面异质性很强的肿瘤,加
软组织肿瘤主要是指一大类源于间叶组织的肿瘤,传统上还包括了周围神经源性的肿瘤,胚胎发生上主要源于中胚层和神经外胚层。腹膜后腔是指位于横膈以下盆膈以上,后壁层腹膜与腹横筋膜间的潜在腔隙,是软组织肿瘤的好发部位之一。
原发性腹膜后肿瘤是指源于腹膜后腔非特定脏器的一大类肿瘤,其中逾半数以上为软组织肉瘤。原发性腹膜后软组织肿瘤(后简称「腹膜后肿瘤」)涵盖了数十种组织学类型和生物学行为方面异质性很强的肿瘤,加之解剖结构的特殊性和多见的巨大瘤体,增加了临床诊治的难度。
由北京大学肿瘤医院软组织和腹膜后肿瘤中心出品的《原发性腹膜后软组织肿瘤诊疗共识》已经发布,本文从诊断、分期、治疗三个方面进行概述该专家共识。
诊断
腹膜后肿瘤的诊断,包括影像学诊断和病理学诊断两部分。
五大目的
1. 评估肿瘤的质地和内部成分、大小、数目、部位、范围、与邻近重要解剖结构的关系,以及可能的病理学类型;
2. 明确是否有远位转移病灶,以及转移病灶的部位、范围、数目、大小等;
3. 评估治疗效果,为进一步治疗方案的调整提供证据;
4. 对拟行手术切除的病人行风险评估;
5. 对经治病人进行随访。
方式
超声、CT、MRI 和 PET-CT,各自的优势与教学书上无异,在此不再赘述,临床可酌情选用。
唯一值得注意的一点是本共识不推荐超声和 PET-CT 单独用于影像学诊断。
对于所有可能接受治愈性手术切除的病人,应尽量避免针吸活检,如若必须应尽量将取材通道选择于手术时可同时切除的部位,并作明确标记。术前活检首选超声或其他影像学引导下芯针穿刺活检术。
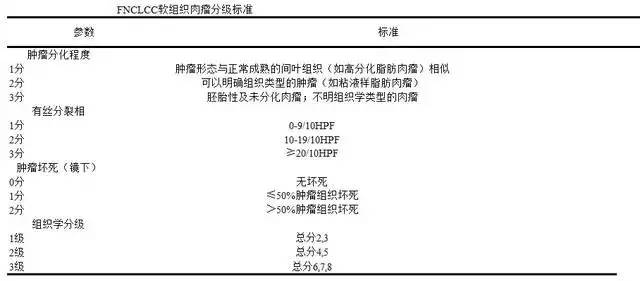
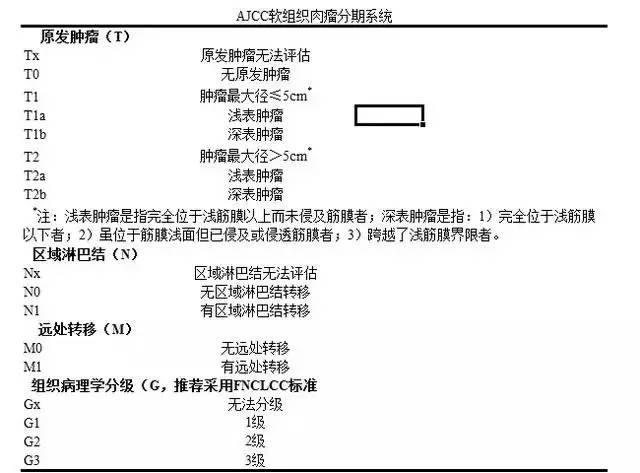
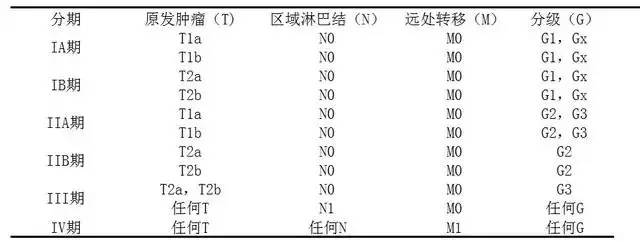
如下表
手术
后腹膜肿瘤的治疗以手术为主,本共识强调,对于结合现有影像学手段和临床资料仍不能判断良恶性的腹膜后肿瘤,均应归类为「良恶性不确定」肿瘤,外科治疗上应遵循后腹膜软组织肉瘤的处理原则。
手术切除尽可能以 R0 切除目标,虽然限于该肿瘤的特殊性,手术范围多依靠术者的判断(术前和术中)、经验和观念来确定。但首次手术 R0 切除毕竟是此类患者获得潜在治愈性疗效的唯一机会。
此外,除了极少部分特定病理学类型(如分化良好的脂肪肉瘤)和特殊情况外,并不推荐对患者行肿瘤姑息性切除。
其他治疗
之所以把化疗、放疗、靶向治疗、生物治疗、免疫治疗、射频消融等等肿瘤治疗手段放在「其他」里,是因为目前除了手术,上述治疗效果仍不明确,并不推荐首选。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腹膜后#
72
#原发性#
64
学习了,好
86
有意思,学习一下
89
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
83
值得学习
68
#软组织#
61
#腹膜#
49
学习了,赞一个!
82
学习了,赞一个!
57