JAMA Netw Open:炎性乳腺癌患者前哨淋巴结活检的趋势
2022-02-12 MedSci原创 MedSci原创
在缺乏高质量随机数据的情况下,SLNB不应用于IBC患者。
炎症性乳腺癌(IBC)是一种侵袭性癌症,占美国每年诊断的所有乳腺癌的1%至6%。IBC是根据继发于乳腺急性炎症变化的临床标准进行诊断的,这种变化导致皮肤淋巴管阻塞并伴有肿瘤栓塞,引起弥漫性红斑和水肿。高达90%的IBC患者可能出现局部淋巴结疾病,其死亡率是非炎症性局部晚期乳腺癌的2倍。
IBC的护理标准是新辅助化疗、全乳房切除术伴腋窝淋巴结清扫(ALND)和乳房切除术后放射治疗。现有研究表明,前哨淋巴结活检(SLNB)在IBC中可能不可靠。SLNB在IBC女性患者中的使用和频率尚不明确。那么,炎性乳腺癌(IBC)患者的前哨淋巴结活检(SLNB)率是多少?在这项研究中,研究者们探讨了美国IBC患者SLNB的频率和时间趋势。

这项回顾性队列研究使用了国家癌症数据库——一个基于全国医院的癌症登记系统,纳入2012年至2017年被诊断为非转移性IBC并接受腋窝手术的女性。数据分析从2021年1月到2021年5月。
这项研究共纳入1096名女性,她们在2012年至2017年间被诊断为非转移性IBC,年龄在18岁或以上。1096名接受SLNB治疗的女性中,186名(17%)为白人,137名(73.7%);1096名女性中有910名(83%)只接受了ALND,其中676名(74.3%)为白人。在接受任何SLNB的女性中,186人中有119人(64%)没有完成ALND。
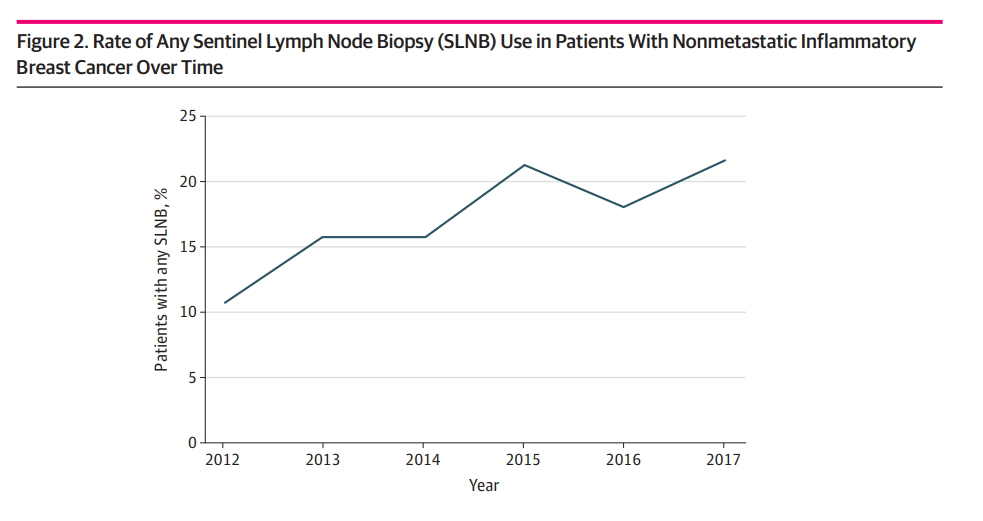
前哨淋巴结活检(SLNB)在非转移性炎性乳腺癌患者中的应用率
从2012年到2017年,SLNB的使用呈统计学显著上升趋势。在多变量分析中,SLNB的使用与诊断年份、临床淋巴结状态和接受重建手术有关。
在这项研究中,研究者使用了代表美国大多数新诊断癌症的医院癌症登记数据,以证明IBC患者中SLNB的使用频繁且不断增加。在IBC患者中使用SLNB是没有循证证据的,也没有当前指南的支持,并且可能代表高度侵袭性癌症治疗的不安全降级。在缺乏高质量随机数据的情况下,SLNB不应用于IBC患者。
参考文献:Sosa A, Lei X, Woodward WA, et al. Trends in Sentinel Lymph Node Biopsies in Patients With Inflammatory Breast Cancer in the US. JAMA Netw Open. 2022;5(2):e2148021. doi:10.1001/jamanetworkopen.2021.48021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
52
#前哨淋巴结活检#
87
#NET#
54
#活检#
86
#淋巴结#
64
#前哨淋巴结#
85
#乳腺癌患者#
70