胆囊内胃粘膜组织异位伴肠上皮化生与中度不典型增生:2例病例报告
2015-03-11 MedSci MedSci原创
图1组织学检查 图1(A)阿尔新蓝(Alcian blue)过碘酸雪夫氏染色(PAS)染色正常(箭头所示)和胆囊上皮化生。肠上皮化生的酸粘蛋白呈蓝色,而胃上皮化生(幽门型)的中性粘蛋白呈红色(X320)。(B)胆囊异位胃粘膜(胃体型),壁细胞(顶部)有一个大的锥体形结构,富含嗜酸性细胞质(苏木素-伊红
图1组织学检查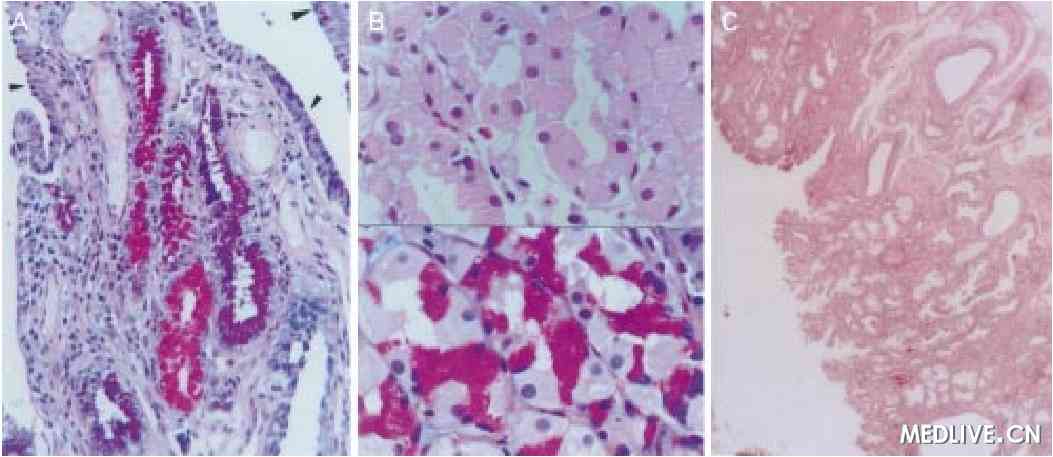 |
|
图1(A)阿尔新蓝(Alcian blue)过碘酸雪夫氏染色(PAS)染色正常(箭头所示)和胆囊上皮化生。肠上皮化生的酸粘蛋白呈蓝色,而胃上皮化生(幽门型)的中性粘蛋白呈红色(X320)。(B)胆囊异位胃粘膜(胃体型),壁细胞(顶部)有一个大的锥体形结构,富含嗜酸性细胞质(苏木素-伊红X480),同一区域(底部)Alcian blue-PAS(X480)染色。(C)胆囊息肉包含异位胃粘膜(苏木素-伊红X180)。
|
 |
|
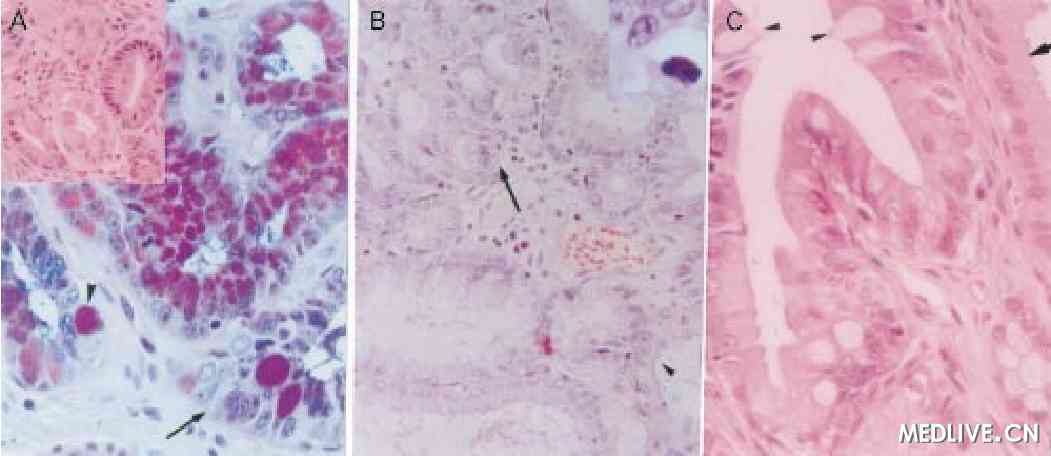
图2(A)上皮细胞轻度及局部中度不典型增生(箭头所示),发生在肠上皮化生(箭头)(Alcian blue-periodic-acid-SchiV (PAS)染色X320)(插图:幽门型化生上皮可见轻度不典型增生(苏木素 - 伊红X320)(B)该区域可见正常(箭头)和化生上皮(箭头)之间的过渡(苏木素 - 伊红X320),轻度不典型增生清晰可辩(插图:苏木素 - 伊红X850)。(C)接近正常胆囊上皮的胆管区可见肠上皮化生(箭头所示)(苏木素 - 伊红X540)。
|
组织学检查,提示结节位于固有层,由异位胃粘膜构成,包括胃体型和幽门型胃腺体,上覆粘膜增生。靠近异位粘膜处可见广泛的幽门腺化生和肠化生(图1A,B)并伴有化生上皮轻度—局部中度的不典型增生改变(图2A - C)。其它部分粘膜呈明显慢性胆囊炎的典型特征。未见胆结石。
超声可清晰显示交界部息肉。行胆囊切除术来治疗胆囊炎和胆囊息肉。胆囊切除标本8x2x0.9cm,可见一层光滑的灰白色浆膜。切开后可见胆囊颈部及胆囊管开口处可见红色-浅灰色息肉样结节,最大直径达0.8cm,其余部分为光滑的天鹅绒样绿色粘膜,厚度为0.4cm。未见胆结石。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








继续学习
77
继续学习
77
#肠上皮化生#
111
#胃粘膜#
73
#不典型增生#
82
#不典型#
63
#粘膜#
63
看起来很厉害的样子
134
这种诊断应该比较困难
143
#病例报告#
61