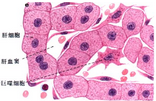
Cell子刊:新方法纯化出史上最纯的肝细胞群体
2016-08-31 佚名 生物谷
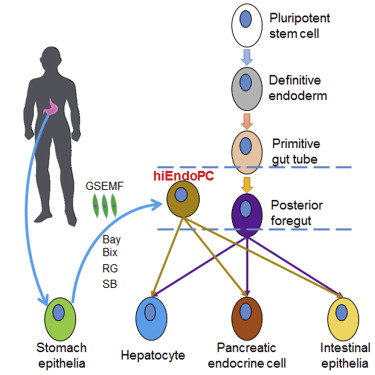
在一项新的研究中,来自美国南卡罗莱纳医科大学和威斯康星医学院的研究人员发现一种更好的方法纯化利用诱导性多能干细胞(ipsC)制造出的肝细胞。这一发现将有助研究肝脏疾病。相关研究结果于2016年8月25日在线发表在Stem Cell Reports期刊上,论文标题为“Mapping the Cell-Surface N-Glycoproteome of Human Hepatocytes Rev
这种新方法可能促进一种重要的临床目标---通过移植利用自己的干细胞产生的未发生突变的肝细胞来治疗肝脏中存在致病性突变的病人---取得突破。之前的利用干细胞产生肝样细胞(liver-like cell)的研究产生异质性的细胞群体,而且这种细胞群体与病人体内的患病肝脏存在很少的类似性。
传统上抗体被用来识别细胞表面上的成熟特征和纯化相似的细胞。这种方法在干细胞研究中是至关重要的,但是可购买的识别成熟肝细胞的抗体比较少,而且往往识别许多不同类型的细胞。在混合细胞群体中的很多细胞类型具有不同的特征,从而可能会遮盖住潜在的致病性的基因突变。
论文通信作者、南卡罗莱纳医科大学发育生物学家Stephen A. Duncan博士说道,“如果没有一种纯的肝细胞群体,就很难找出这些基因突变导致的相对微妙的差异,但是这些差异在一个人的一生当中起着重要的作用。”
为了不依赖抗体,Duncan和同事们采取一种被称作化学蛋白质组细胞表面捕获(chemoproteomic cell surface capture, CSC)的新技术。标记的细胞要比未标记的细胞具有更加类似的成熟肝细胞特征。未发生分化的多能性干细胞被排除在标记的细胞群体之中。
Duncan说,“这是比较重要的。如果你想要将细胞移植到患有肝脏疾病的病人体内,那么你肯定不想要也将多能性干细胞移植到病人体内,这是因为多能性干细胞会形成畸胎瘤。”
Duncan提醒道,迄今为止,移植利用iPSC产生的干细胞还未准备转化到诊所临床实践当中。但是如今,这种分选同质的肝细胞的技术能够被用来在细胞培养皿中成功地和准确地建立疾病模型和研究疾病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
33
#新方法#
46
#Cell#
34
#肝细胞#
36
#群体#
45
学习起来
0