Cell:研究发现白血病关键信号机制AKT/FOXO
2011-10-18 MedSci原创 MedSci原创
来自麻省总医院再生医学研究所,哈佛大学等处的研究人员发现了白血病中一种关键信号机制,提出了AKT/FOXOs之前未知的新功能,为不同基因型的白血病患者的治疗提出新的思路。这一研究成果公布在《细胞》(Cell)杂志上。 文章的通讯作者是哈佛大学干细胞研究所共同所长David T. Scadden博士,这位著名的研究人员被列入了当今干细胞研究方面的顶尖科学家,作为干细胞研究的中青年骨干,Scadde
来自麻省总医院再生医学研究所,哈佛大学等处的研究人员发现了白血病中一种关键信号机制,提出了AKT/FOXOs之前未知的新功能,为不同基因型的白血病患者的治疗提出新的思路。这一研究成果公布在《细胞》(Cell)杂志上。
文章的通讯作者是哈佛大学干细胞研究所共同所长David T. Scadden博士,这位著名的研究人员被列入了当今干细胞研究方面的顶尖科学家,作为干细胞研究的中青年骨干,Scadden博士专长于干细胞分化再生的微环境调控机理的研究。
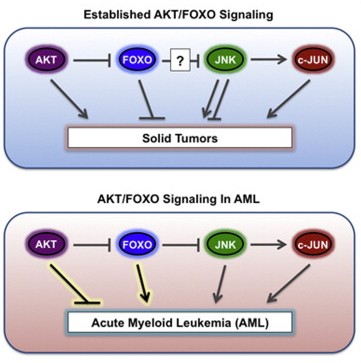
AKT也称为蛋白激酶B(PKB),是一种相对分子质量为60 000的丝氨酸/苏氨酸激酶,这种蛋白与许多恶性肿瘤相关,能通过部分抑制FOXO肿瘤抑制因子参与肿瘤发生。在这篇文章中,研究人员发现了急性髓系白血病AML中AKT/FOXOs的一种新型可逆作用,为进一步研究AML机制,以及癌症信号通路提出了新见解。
急性髓系白血病AML是一种原发于骨髓异常血细胞快速生长的侵袭性癌症,其发病率随着人的年龄而增加。AML最常见的症状是体重减轻、疲乏、发热、盗汗和纳差,这种疾病可以扩散浸润到机体的其他部位如淋巴结、肝和脾。
在这篇文章中,研究人员分析了多位AML病患,发现无论其基因型是什么,四成的AML病患中FOXOs都被激活了,这与之前的研究发现相悖。通过进一步实验,研究人员又发现AML确实与其它癌症不同,它需要低表达量AKT,及高表达量FOXO。而且FOXO的这种活性还与JNK/c-JUN信号途径有关,这些实验数据都表明了AKT/FOXO,以及JNK/c-JUN信号途径在维持分化壁垒方面的重要作用,这种壁垒能用于靶向抑制白血病,这将为不同基因型的白血病患者的治疗提出新的思路,也有助于科学家们深入分析白血病中的信号通路。
除此之外,Scadden博士研究组近期还在Nature Biotechnology杂志上,报道了分离干细胞与其他的造血细胞和肿瘤细胞的新方法。他们将外周血单核细胞(PBMCs)置入脉冲电场中,单核细胞可被选择性地剔除,而一些小的淋巴细胞则可以保留下来,这些小的淋巴细胞尚存在功能,并可以通过离心将他们与死亡细胞分离。
研究人员首先将PBMCs与肿瘤细胞混合,然后将混合物置入电场后,发现肿瘤细胞也能够被选择性地剔除。而且,将一种可移植的肿瘤细胞置入电场后再植入免疫缺陷小鼠,未见肿瘤发生。最后,研究人员将外周血干细胞置入电场进行研究,结果发现,该方法可以增加CD34-阳性/CD38-阴性的干细胞,同时保持其功能。这种方法与利用抗体进行纯化的细胞分离技术相比较,该系统需要的试剂较少,因此其费用较低。对于那些需要进行移植的恶性血液病患者来说,该方法是分离纯化以及获得干细胞的最佳途径。
原始出处:
doi:10.1016/j.cell.2011.07.032
PMC:
PMID:
AKT/FOXO Signaling Enforces Reversible Differentiation Blockade in Myeloid Leukemias
Stephen M. Sykes, Steven W. Lane, Lars Bullinger, Demetrios Kalaitzidis, Rushdia Yusuf, Borja Saez, Francesca Ferraro, Francois Mercier, Harshabad Singh, Kristina M. Brumme, Sanket S. Acharya, Claudia Scholl, Zuzana Tothova, Eyal C. Attar, Stefan Fröhling, Ronald A. DePinho, D. Gary Gilliland, Scott A. Armstrong, David T. Scadden
AKT activation is associated with many malignancies, where AKT acts, in part, by inhibiting FOXO tumor suppressors. We show a converse role for AKT/FOXOs in acute myeloid leukemia (AML). Rather than decreased FOXO activity, we observed that FOXOs are active in 40% of AML patient samples regardless of genetic subtype. We also observe this activity in human MLL-AF9 leukemia allele-induced AML in mice, where either activation of Akt or compound deletion of FoxO1/3/4 reduced leukemic cell growth, with the latter markedly diminishing leukemia-initiating cell (LIC) function in vivo and improving animal survival. FOXO inhibition resulted in myeloid maturation and subsequent AML cell death. FOXO activation inversely correlated with JNK/c-JUN signaling, and leukemic cells resistant to FOXO inhibition responded to JNK inhibition. These data reveal a molecular role for AKT/FOXO and JNK/c-JUN in maintaining a differentiation blockade that can be targeted to inhibit leukemias with a range of genetic lesions.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
61
#研究发现#
60
#Akt#
54
#CEL#
52
希望对治疗有用
164