Lancet Haematol:间充质干细胞治疗改善激素耐药的急性GVHD患者生存
2015-11-30 MedSci MedSci原创
注射MSCs是治疗激素耐药的急性GVHD的一个可行的治疗方法。迫切需要随机临床试验评估不同治疗方法对激素耐药的急性移植物抗宿主病的效果。
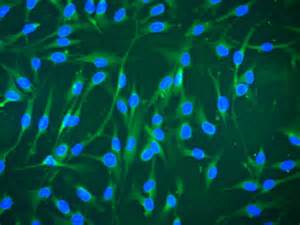
背景:GVHD(Graft-versus-host disease ,移植物抗宿主病)是HSCT(allogeneic haemopoietic stem-cell transplantation,同种异体造血干细胞移植)的主要限制,目前尚无切实可用的治疗方法。在一些欧洲国家使用MSCs(mesenchymal stromal cells,间充质干细胞)已经成为标准治疗GVHD方法,但是对于患者接受MSCs的受益,目前尚存争议。本Meta分析的目的是分析现有证据,说明MSC治疗激素耐药的急性GVHD的受益。
方法:系统回顾和荟萃分析,评估激素耐药的急性GVHD患者行MSC治疗的反应和生存。搜索MEDLINE、Embase、Ovid和Cochrane Central数据库中已发表的研究,ClinicalTrials.gov和其他网站中未发表的临床试验和会议文献摘要。研究类型包括前瞻性和回顾性研究,干预方法是激素耐药的急性GVHD患者接受MSCs。由两个独立调查人员根据严格的选择标准提取数据。使用随机效应模型分析各项研究的预后。
主要指标:急性GVHD患者初次注射MSCs后6个月生存率。
结果:研究共发现628项文献,阅读文献后排除610项文献,有5项文献没有包含相关数据。因此,Meta分析包括13项包含中度不完整偏倚的非随机研究,共有336名患者。
六项研究提供的数据包含主要结果分析(119名患者)。在MSC治疗后6个月生存率为63%(95%CI 50-74,I2=41%)。生存率与患者年龄、MSC培养基或MSC剂量无关。
结论:现有证据表明注射MSCs是治疗激素耐药的急性GVHD的一个可行的治疗方法。迫切需要随机临床试验评估不同治疗方法对激素耐药的急性移植物抗宿主病的效果。
原始出处:
Hashmi,Shahrukh, et al. Survival after mesenchymal stromal cell therapy in
steroid-refractory acute graft-versus-host disease: systematic review and meta-analysis.The Lancet Haematology. Published Online 26 November 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









感谢分享一下!
79
感谢分享一下!
98
#患者生存#
51
#HAE#
62
#间充质干细#
53
#Lancet#
62
好文章
144
应用于临床还需实践检验
133
#EMA#
75
观望
174