Nat Commun:肿瘤—睾丸基因表达模式有助于揭开肿瘤发生的秘密
2016-01-31 MedSci MedSci原创
<div class="p1Textcen font14" id="Zoom"><p>来自南京医科大学的研究人员报告称,他们在19种<span class="tip_s">癌症</span>类型中系统鉴别了呈肿瘤—睾丸(Cancer-testis,CT)基因表达模式的基因。他们的研究成果发布在1月27日的《自然通讯》(Nature Communications)杂志上。<span style="font-size: 9pt;">南京医科大学的</span>胡志斌(Zhibin Hu)教授、沙家豪(Jiahao Sha)教授和沈洪兵(Hongbing Shen)是这篇论文的共同通讯作者。</p><p>肿瘤—睾丸(Cancer-testis,CT)基因表达模式指提原本仅仅在睾丸系统(生殖系统)表达的特异性基因,在肿瘤细胞中同样也呈现表达,是近年来研究的关注热点之一。<span style="text-indent: 28px;">肿瘤-睾丸抗原(Cancer-testis antigen,CTA)是一类具有特异性表达模式的肿瘤相关抗原,具有加速肿瘤形成,抵抗肿瘤细胞凋亡。类似基因如</sp
来自南京医科大学的研究人员报告称,他们在19种癌症类型中系统鉴别了呈肿瘤—睾丸(Cancer-testis,CT)基因表达模式的基因。他们的研究成果发布在1月27日的《自然通讯》(Nature Communications)杂志上。南京医科大学的胡志斌(Zhibin Hu)教授、沙家豪(Jiahao Sha)教授和沈洪兵(Hongbing Shen)是这篇论文的共同通讯作者。
肿瘤—睾丸(Cancer-testis,CT)基因表达模式指提原本仅仅在睾丸系统(生殖系统)表达的特异性基因,在肿瘤细胞中同样也呈现表达,是近年来研究的关注热点之一。肿瘤-睾丸抗原(Cancer-testis antigen,CTA)是一类具有特异性表达模式的肿瘤相关抗原,具有加速肿瘤形成,抵抗肿瘤细胞凋亡。类似基因如TSP50,ssx1,NY-ESO-1,CT45-5,CAGE,MAGE等。
肿瘤—睾丸基因的存在反映了精子发生(spermatogenesis)与肿瘤发生(tumorigenesis)之间的相似性。有可能它们的选择性表达模式可以帮助鉴别出癌症中的一些驱动基因。
在这项新研究中,南京医科大学的研究人员整合了来自多个数据库的转录组数据,在19个癌症类型中系统鉴别出了876个新的CT基因。他们探讨了这些基因与睾丸特异性调控元件(TSREs)之间的关系。提出了极端高水平表达的CT基因(EECTGs)是可以通过一些表观遗传机制激活的潜在驱动子。
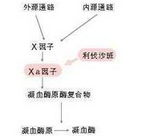
研究人员发现了EECTGs与一些突变基因,如乳腺癌中PIK3CA基因的体细胞突变之间呈相互排斥关系。他们还提供了证据表明,启动子去甲基化和附近的非编码RNAs(CT-ncRNAs)可能是重新激活EECTG基因表达的两种机制。并证实了减数分裂相关EECTG (MEIOB)和邻近的CT-ncRNA在肺腺癌肿瘤发生中发挥作用。
新研究扩展了我们对于CT基因的认识,并为我们鉴别癌症中的表观遗传驱动基因提供了新思路,在未来这些表观遗传基因有可能成为癌症治疗的靶点。
胡志斌、沙家豪和沈洪兵三位教授近年来在各自的研究领域取得了不少骄人的研究成果。
原始出处:
Wang C, Gu Y, Zhang K, Xie K, Zhu M, Dai N, Jiang Y, Guo X, Liu M, Dai J, Wu L, Jin G, Ma H, Jiang T, Yin R, Xia Y, Liu L, Wang S, Shen B, Huo R, Wang Q, Xu L, Yang L, Huang X, Shen H, Sha J, Hu Z.Systematic identification of genes with a cancer-testis expression pattern in 19 cancer types. Nat Commun. 2016 Jan 27;7:10499. doi: 10.1038/ncomms10499.
相关文献:
Zhong J, Chen Y, Liao X, Li J, Wang H, Wu C, Zou X, Yang G, Shi J, Luo L, Liu L, Deng J, Tang A.Testis expressed 19 is a novel cancer-testis antigen expressed in bladder cancer. Tumour Biol. 2015 Dec 22
Ghafouri-Fard S.Expression of cancer-testis antigens in stem cells: is it a potential drawback or an advantage incancer immunotherapy. Asian Pac J Cancer Prev. 2015;16(7):3079-81.
Ghafouri-Fard S.Expression of Cancer-Testis Antigens in Pediatric Cancers. Asian Pac J Cancer Prev. 2015;16(13):5149-52.
作者简介:
胡志斌教授:教育部***特聘教授和国家基金委杰出青年基金获得者,现任生殖医学国家重点实验室副主任,南京医科大学公共卫生学院副院长。主持科技部青年“973”项目、自然科学基金重大项目课题等多项。在Nature Genetics,J Clin Invest,J Clin Oncol等专业杂志上发表论文200多篇,SCI他引超过5000次。
沙家豪博士,男,1959年5月出生,南京医科大学特聘教授,博士生导师,生殖医学国家重点实验室主任和“配子发生的分子机制”学术带头人,科技部 “生殖与发育重大科学计划”专家组成员、“生殖健康的基础和临床研究”教育部创新团队带头人、国家杰出青年科学基金获得者、中国动物学会生殖生物学分会副理事长、江苏省解剖学会理事长、江苏省细胞遗传学会副理事长、《Asian J Androl》编委、《Chinese Science Bulletin》编委、《生殖医学杂志》常务编委、《中国男科杂志》编委、《男科学报》编委、《中国计划生育学杂志》编委和《国外医学》计划生育分册常务编委;在国内外SCI收录杂志发表论文70篇。
沈洪兵博士, 男,1964年5月出生,南京医科大学特聘教授,博士生导师。生殖医学国家重点实验室副主任,教育部“***”特聘教授,国家杰出青年科学基金获得者,新世纪百千万人才工程国家级人选,全国百篇优秀博士论文指导教师。现任国际肿瘤和分子流行病学专业期刊《Lung Cancer》、《Oncology Reports》、《International Journal of Molecular Epidemiology and Genetics》等杂志编委,并为《J Clin Oncol》、《Gut》、《Cancer Res》等10多个国际杂志审稿人。主要致力于环境与肿瘤的分子流行病学研究,作为通讯/第一作者发表SCI论文100余篇。作为第一完成人先后获教育部高校自然科学奖一等奖,江苏省科技进步二等奖及中华医学科技进步二等奖等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
55
#Nat#
75
那女生岂不是很尴尬。
176
#基因表达#
83
#睾丸#
80
收藏
173