Eur J Cancer:来那替尼(Neratinib)延伸辅助治疗在HER2/HR共阳性早期乳腺癌患者的疗效和安全性分析:来自德国ExteNET研究的亚组分析结果
2021-05-23 yd2015 MedSci原创
来那替尼(neratinib)的延伸辅助治疗可以使HER2和HR共阳性的早期乳腺癌患者临床获益。
人类生长因子受体2(HER2)阳性的早期乳腺癌(EBC)约占13-20%,在没有抗HER2治疗之前,HER2阳性的乳腺癌患者较HER2阴性的患者预后较差。虽然目前抗HER2的治疗能够明显改善患者的预后,但是治疗后的复发率仍很高。而且在HER2阳性和激素受体(HR)阳性的患者中,抗HER2的治疗疗效会打折扣。因此,有必要寻找能够降低复发率的治疗。来那替尼(Neratinib)是一种泛HER治疗的TKI。根据来那替尼的结构等特点,已有研究发现其可逆转曲妥珠单抗、帕妥珠单抗的耐药。目前已被欧盟批准用于共阳性EBC患者完成术后辅助治疗后的延伸辅助治疗。而且,III期临床试验ExteNET已经表明,总体人群中来那替尼的延伸辅助治疗对比安慰剂可明显改善患者预后,2年的无进展率为93.9 vs. 91.6%; HR=0.67,95%CI(0.50-0.91); p = 0.0091。近期,研究者在European Journal of Cancer杂志上发表了来自ExteNET试验中HER2和HR共阳性早期乳腺癌患者来那替尼的疗效和安全性。
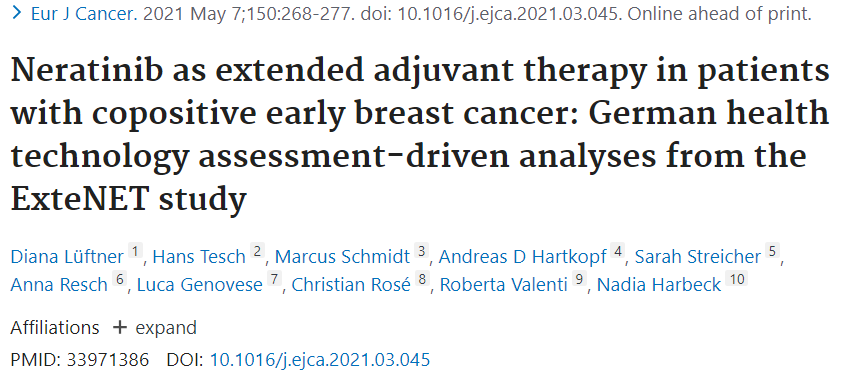
HER2和HR共阳性的患者为1631例,其中来那替尼组为816例,安慰剂组为815例。中位治疗时间分别为11.5和11.9个月。
两组的临床特征
中位随访时间为2年时,来那替尼较安慰剂明显延长无病进展期(DFS),2年的DFS率分别为95.6和91.5%(HR=0.45,95%CI [0.29-0.69]; p =0.0002);同样,来那替尼较安慰剂明显延长远处无病进展期(DDFS),2年DDFS率分别为96.4和93.3%(HR=0.52,95%CI [0.32-0.84]; p= 0.0082)。5年中位随访时间时,来那替尼和安慰剂的5年DFS率分别为91.2和86.8%(HR= 0.57,95%CI [0.41-0.78]; p= 0.0005);5年的DDFS率分别为92.7和88.7%(HR=0.60,95%CI [0.42-0.85];P=0.0037)。

两组2年的DFS和DDFS
生活质量分析,两组的治疗并没有明显差异。治疗1个月,肿瘤治疗功能评估总体评分显示两组有明显差异。不良事件(AE)分析发现来那替尼组治疗在任何级别的AE,严重的AE和AE导致治疗的中断等方面明显高于安慰剂中。来那替尼的不良事件主要为胃肠道事件(任何级别/III级),为腹泻(94.4/39.4%);恶心(43.9/1.6%); 呕吐(26.6/3.2%); 腹痛(23.8/1.9%)和疲劳(28.1/1.9%)。来那替尼组发生IV级和V级不良事件比例分别为1.0% (n =8)和0.1% (n = 1) ,而安慰剂组分别为0.6% (n = 5) 和0%。没有累计或不可逆的毒性发生。

治疗相关不良事件
综上,来那替尼(neratinib)的延伸辅助治疗可以使HER2和HR共阳性的早期乳腺癌患者临床获益。基于此,德国已经批准这一治疗策略。
原始出处:
Diana Lüftner, Hans Tesch, Marcus Schmidt, et al. Neratinib as extended adjuvant therapy in patients with copositive early breast cancer: German health technology assessment-driven analyses from the ExteNET study. Eur J Cancer. 2021 May 7;150:268-277. doi: 10.1016/j.ejca.2021.03.045. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#NET#
77
#疗效和安全性#
93
#ERA#
74
#德国#
71
#乳腺癌患者#
76
谢谢梅斯提供这么好的信息,学到很多
81
延伸辅助
138