BMJ:多药疗法背景下阿哌沙班与华法林治疗房颤的疗效比较(ARISTOTLE)
2016-06-17 Seven L 译 MedSci原创
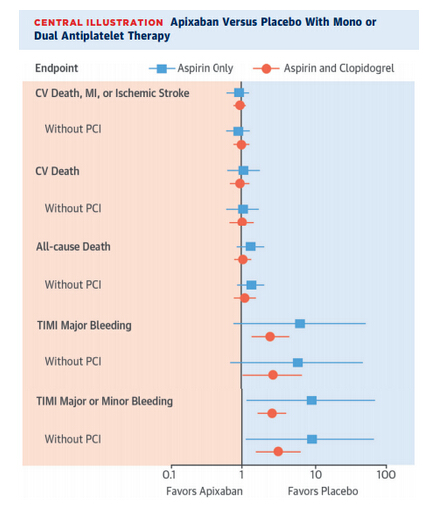
研究者对ARISTOTLE(2006-2011年,多中心、双盲、双模拟试验,阿哌沙班可减少房颤患者卒中和其他血栓栓塞事件风险)研究结果进行了事后分析,涉及18201名参与者,探究越来越多的伴随药物背景下,阿哌沙班和华法林对房颤治疗的差异。ARISTOTLE试验中患者被随机分为每天2次5 mg阿哌沙班组(n=9120)或华法林组(以国际标准化比值范围2.0-3.0为目标;n = 9081)。事后分析
研究者对ARISTOTLE(2006-2011年,多中心、双盲、双模拟试验,阿哌沙班可减少房颤患者卒中和其他血栓栓塞事件风险)研究结果进行了事后分析,涉及18201名参与者,在越来越多的伴随药物背景下,探究阿哌沙班和华法林对房颤治疗的差异。ARISTOTLE试验中患者被随机分为每天2次5 mg阿哌沙班组(n=9120)或华法林组(以国际标准化比值范围2.0-3.0为目标;n = 9081)。事后分析中根据患者在基线时的伴随药物数目(0-5, 6-8, ≥9)进行分层分析,中位数随访1.8年。校正年龄、性别和国家等因素后,以阿哌沙班和华法林对临床预后和治疗效果为主要检测指标。数据显示,平均每位患者伴随了6种药物(范围5-9);≥5种药物的多药疗法见于13932(76.5%)名患者。更多数目的伴随药物主要见于老年人、女性和美国的患者。分层分析显示,随着伴随药物的增加,并发症和死亡率也显著增加(P<0.001),卒中或全身性栓塞发生率在伴随药物0-5、6-8和≥9种中分别为1.29、1.48和1.57/100人-年;主要出血的发生率分别为1.91、2.46和3.88/100人-年。无论
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#药疗法#
79
#BMJ#
66
己拜读,受益匪浅
98
深度好文,值得学习,赞!
114
#ARISTOTLE#
56
好文章,值得学习
198