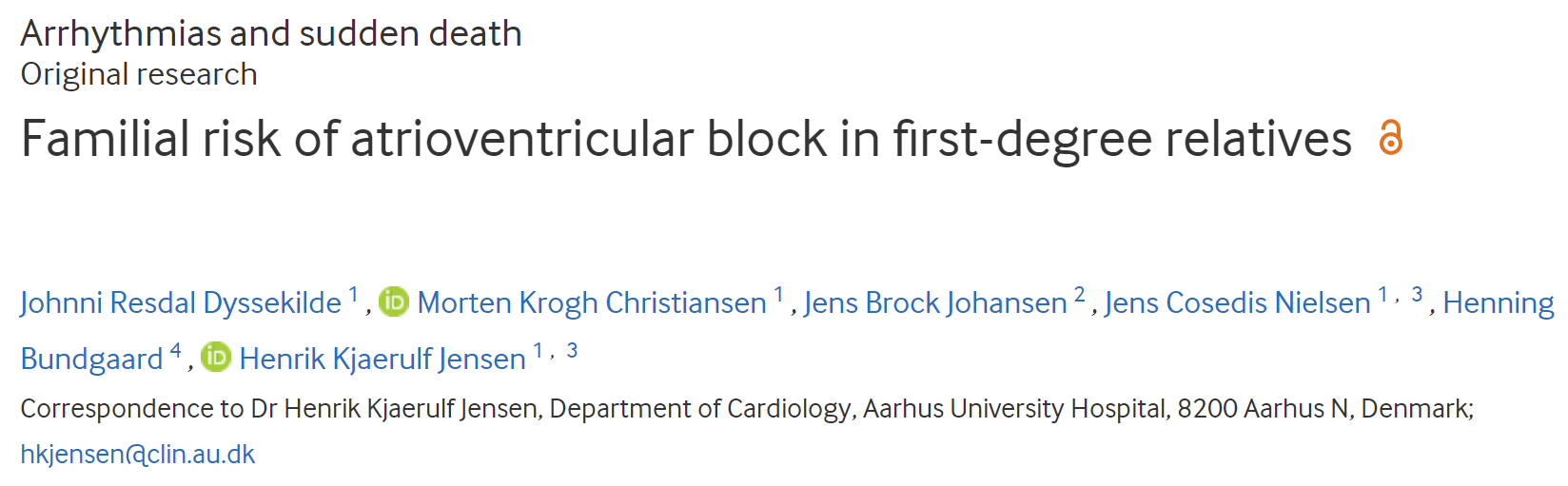
Heart:一级亲属房室传导阻滞的家族风险
2022-03-09 MedSci原创 MedSci原创
房室传导阻滞患者的一级亲属发生房室传导阻滞的风险增加,该风险与起搏器植入时指示病例的年龄呈负相关。这些结果表明,在患有早发性疾病的家庭中,房室传导阻滞的发生存在遗传因素。
房室传导阻滞是最常见的起搏器植入指征,随着年龄的增长,房室传导阻滞的发生率有所增加。在过去十年中,丹麦每年平均每百万居民中有350人因房室传导阻滞而接受了首次起搏器。近年来,有研究报道了罕见的遗传性房室传导阻滞(房室传导阻滞)病例;然而,房室传导阻滞的遗传特性仍然未知。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在评估房室传导阻滞的遗传特性。
研究人员使用了来自丹麦民事登记处的数据,建立了一个全国性的具有父母联系的个人队列。研究人员将数据与来自丹麦起搏器和植入式心脏复律除颤器登记处的信息进行合并,其中包含研究期间在丹麦进行的所有起搏器植入信息,以确定因房室传导阻滞而首次接受起搏器的患者。
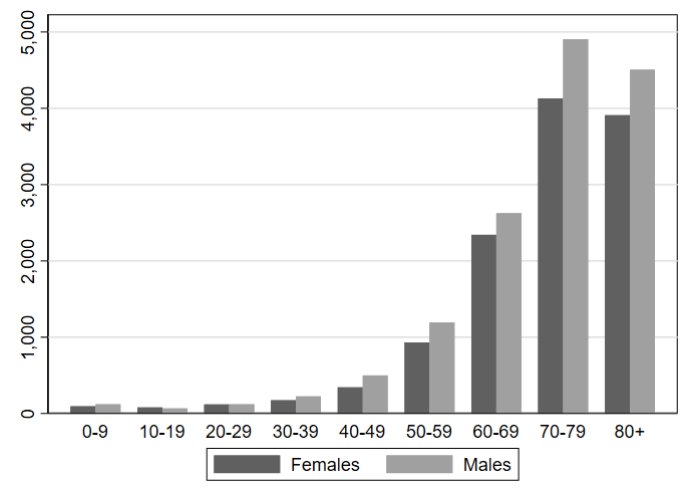
该研究共有4648204名受试者伴有父母联系数据,共有26880名连续就诊患者因房室传导阻滞接受了首次起搏器。总体而言,与一般人群的风险相比,如果父亲、母亲或兄弟姐妹患有房室传导阻滞,则因房室传导阻滞植入起搏器的调整率比(RR)为2.1(95%CI为1.8至2.5)。对于患有房室传导阻滞的母亲的后代,调整后的RR为2.2(1.7-2.9),对于患有房室传导阻滞的父亲的后代,调整后的RR为2.2(1.5-2.4),对于患有房室传导阻滞的患者的兄弟姐妹,调整后的RR为3.5(2.3-5.4)。在植入起搏器时,风险与指示病例的年龄成负相关。如果母亲或父亲在50年前植入起搏器,则相应的调整后RR分别为15.8(4.8-52.3)和10.0(3.3-30.4)。
由此可见,房室传导阻滞患者的一级亲属发生房室传导阻滞的风险增加,该风险与起搏器植入时指示病例的年龄呈负相关。这些结果表明,在患有早发性疾病的家庭中,房室传导阻滞的发生存在遗传因素。
原始出处:
Johnni Resdal Dyssekilde.et al.Familial risk of atrioventricular block in first-degree relatives.heart.2022.https://heart.bmj.com/content/early/2022/03/03/heartjnl-2021-320411
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#房室传导阻滞#
71
#传导阻滞#
76
#ART#
55
#HEART#
0
#一级亲属#
70