AIM:维生素D和钙抑制开始抗逆转录病毒治疗时的骨密度损失
2015-06-17 崔倩 译 MedSci原创
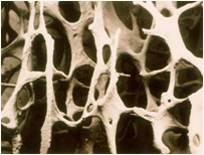
背景:HIV-1感染的起始抗逆转录病毒治疗与骨密度(BMD)损失2%到6%相关。 意义:评估维生素D3加钙的补充对起始抗逆转录病毒治疗相关的骨损失的影响。 设计:48周的前瞻性、随机、双盲、安慰剂对照研究。包括39个艾滋病临床试验组单位。参与者为使用抗逆转录病毒治疗的感染HIV的成人患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗逆转录病毒#
52
#逆转录#
60
#逆转录病毒#
63
内容很新颖,赞
123
如果数据能够更加准确就好了
124
这篇文章不错
153
#转录#
64
bmd应该是个不错的点
126
看看
127
有意思
130