老年男性反复胸闷咳嗽,症状刚有好转便卷土重来,由慢性重度嗜酸粒细胞增多和肺部浸润发现了哪些诊断治疗新认识?
2018-12-14 李强 朱晓萍 等 呼吸界
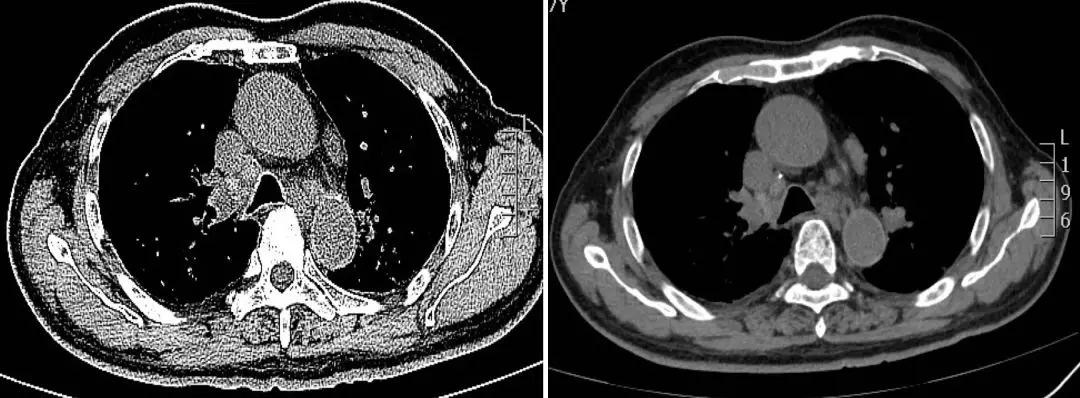
病例回顾男性,77岁,以反复咳嗽胸闷10月,加重半月收住。患者于2018年3月无诱因干咳、胸闷,查血常规:嗜酸性粒细胞4.12 x 10^9/L,E% 41.21%,入住我院血液科行骨穿并基因检测等排除血液系统恶性疾病后考虑继发性嗜酸性细胞增多症,予地塞米松20mg 静滴4d嗜酸性粒细胞降至正常,并症状好转后停用。2018年4月9日,复查嗜酸性粒细胞5.78 x 10^9 /L,再次予以地塞米
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#卷土重来#
60
#老年男性#
54
#胸闷#
52
#诊断治疗#
77
学习
95
好
72