Ann Rheum Dis:骨软骨界面的水平裂隙:肥胖相关性骨关节炎的新型病理特征
2020-04-14 xiangting MedSci原创
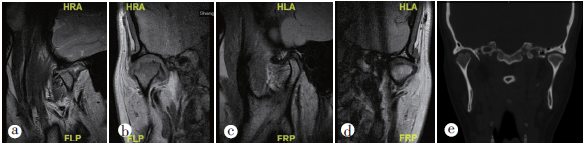
肥胖OA患者的关键病理特征是骨软骨界面的水平裂隙。肥胖与初次TKR的年轻化密切相关,这可能是水平裂隙引起的。
肥胖是公认的骨关节炎(OA)危险因素。这项研究目的是表征骨软骨中与体重指数(BMI)相关的病理变化,并确定肥胖是否是OA患者早期关节置换的主要原因。
研究人员分析了澳大利亚骨科协会国家关节置换登记41023名患者的BMI与接受全膝关节置换(TKR)时年龄之间的相关性。然后分析了登记的一个代表性子集中,BMI对膝关节胫骨平台病理变化的影响。
在澳大利亚,57.58%的TKR患者患有肥胖。超重、I级和II级肥胖或III级肥胖患者分别比体重正常患者早1.89、4.48和8.08年进行TKR。显微镜检查显示,骨软骨界面的水平裂隙是肥胖相关性OA的主要病理特征。水平裂隙的发生率与BMI升高密切相关。BMI每增加1单位(1kg/m2),水平裂隙的几率增加14.7%。84.4%的水平裂隙归因于肥胖。软骨退化的降低和软骨下骨微结构的改变也与BMI升高有关。
肥胖OA患者的关键病理特征是骨软骨界面的水平裂隙。肥胖与初次TKR的年轻化密切相关,这可能是水平裂隙引起的。
原始出处:
Lianzhi Chen. Horizontal fissuring at the osteochondral interface: a novel and unique pathological feature in patients with obesity-related osteoarthritis. Ann Rheum Dis. April 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨软骨#
75
#病理特征#
77
#骨关节#
66
#相关性#
58
#Dis#
68
#关节炎#
51