2016脑梗死研究一览
2016-08-29 MedSci MedSci原创
脑梗死是最常见的脑卒中类型,是由各种原因所致的局部脑组织血液供应障碍,导致脑组织缺血缺氧性病变坏死,进而产生相应的神经功能缺失表现。大面积脑梗死也称恶性大脑中动脉梗死,是导致人类死亡或残疾的重要疾病。此类患者具有较典型的临床症状,相对单一的进程,常常因小脑幕切迹疝而死亡。近期,在美国心脏协会/美国卒中协会(American heart association/American stroke a
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










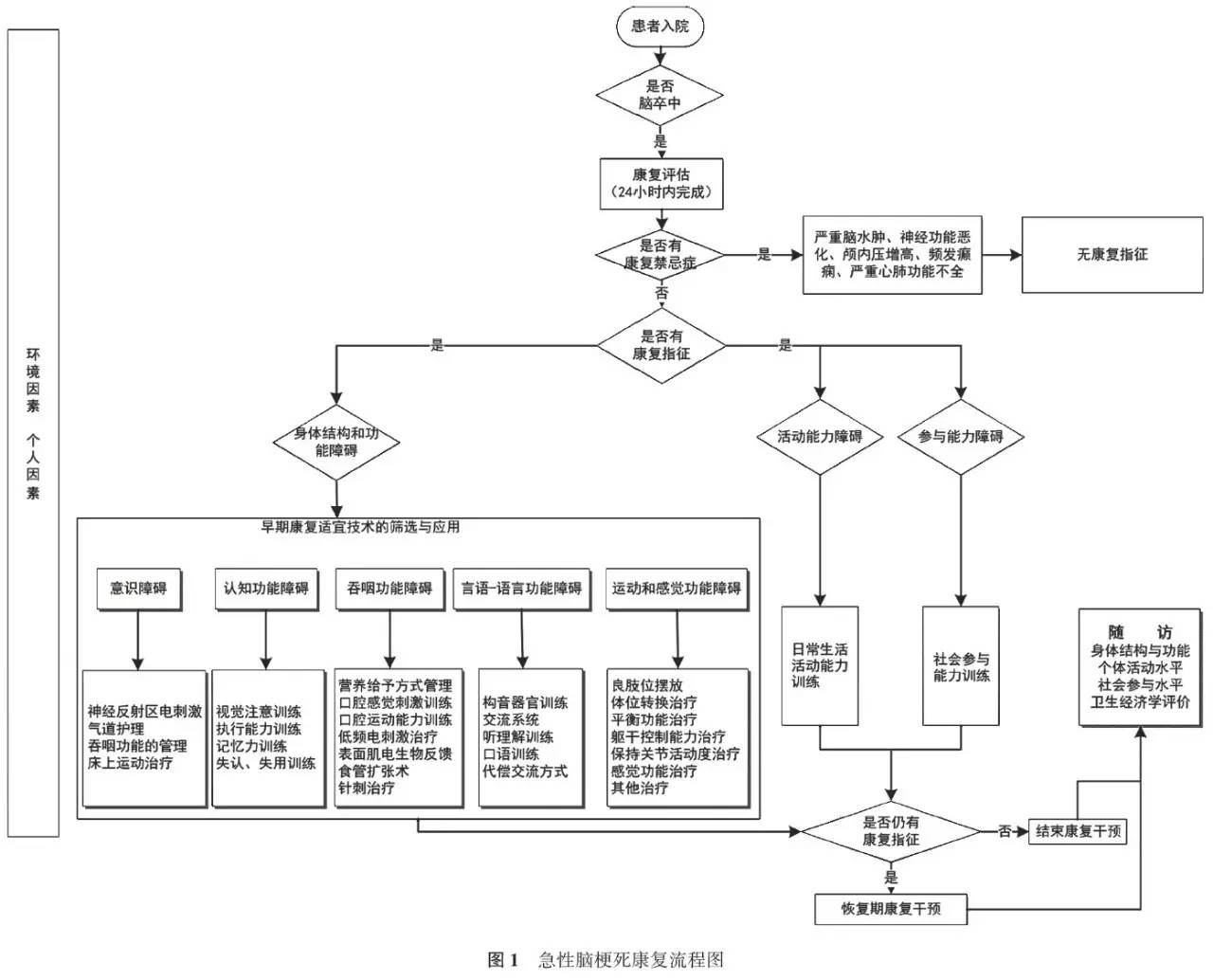
流程图如果能放大就太好了
171
文章很好值得关注
98
学习了,赞一个!
131
#脑梗#
69
学习了啊
132
哎研究更新的太快了
122