NEJM:粘膜和手指黑色素瘤转移-病例报道
2020-07-09 MedSci原创 MedSci原创
该患者接受了dabrafenib和曲美替尼治疗,在5个月的随访中观察到了病灶的部分消退。
患者为一名47岁的男子,因多发指甲,口腔和阴茎病变病史,伴有发热、食欲下降和恶心10天,而到皮肤科门诊就诊。他的病史主要有胸部皮肤黑色素瘤,该皮肤癌已于11年前通过手术切除术进行了治疗。
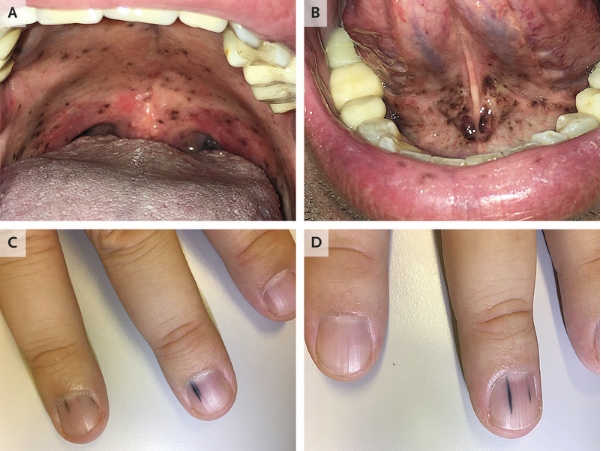
体格检查发现硬腭、软腭以及舌头下方有多个离散的色素性病变(如图A和图B所示)。他的阴茎上也有类似的病变。手部检查显示多个手指的指甲床上有许多纵向黑线(如图C和D所示)。对这些病变的活检证实存在黑色素瘤细胞,这一发现与粘膜和舌状黑色素瘤转移的诊断相一致。
医务人员对患者胃肠道症状开展进一步评估发现胃转移,并通过分子分析鉴定了BRAF突变。
该患者接受了dabrafenib和曲美替尼治疗,在5个月的随访中观察到了病灶的部分消退。
原始出处:
Maria Parodi,et al.Eruptive Mucosal and Ungual Melanoma Metastases.N Engl J Med 2020;https://www.nejm.org/doi/full/10.1056/NEJMicm1915587
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#色素#
50
#粘膜#
59
#黑色素#
58
#黑色素#
61
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
74