陕西一医院26人感染丙肝 医务人员违规操作致院感
2016-02-25 曾春 华商网
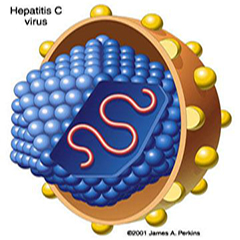
2月17日至19日,镇安县医院在对该院部分血液透析患者例行病毒抗体检测时,发现有患者丙肝病毒抗体阳性,随即将该院相关透析患者血液样本送往省级医院检查,截至2月24日,经会诊,初步确认丙肝病毒感染者26名。 事件发生后,陕西省卫计委派出了专家指导组,市县迅速成立处置工作领导小组,全面展开处置工作,在专家组指导下,立即对镇安县医院相关科室进行整改,严格透析室诊疗制度和操作规范,紧急调配增加透析设备,
2月17日至19日,镇安县医院在对该院部分血液透析患者例行病毒抗体检测时,发现有患者丙肝病毒抗体阳性,随即将该院相关透析患者血液样本送往省级医院检查,截至2月24日,经会诊,初步确认丙肝病毒感染者26名。
事件发生后,陕西省卫计委派出了专家指导组,市县迅速成立处置工作领导小组,全面展开处置工作,在专家组指导下,立即对镇安县医院相关科室进行整改,严格透析室诊疗制度和操作规范,紧急调配增加透析设备,实行分区诊治,对感染患者与非感染患者分离透析,确保透析安全,对已确诊的丙肝病毒感染者,制定诊疗方案,实行免费治疗,积极普及丙肝医学知识,流行病学调查同步展开。
经专家组初步调查分析,此次感染是由于少数医务人员违反操作规程,而导致的一起院内感染事件,目前,已启动调查问责机制,各项处置工作正在进行中。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#违规#
59
悲哀
128
院感若是不注意,随时引发大问题
119
罚
154
值得警惕
158
#院感#
46
#医务人员#
61
唉
148
院感很中要呀
71
小心
81