CLIN CANCER RES:成纤维细胞亚型调节乳腺导管癌对雌激素的反应
2017-04-08 MedSci MedSci原创
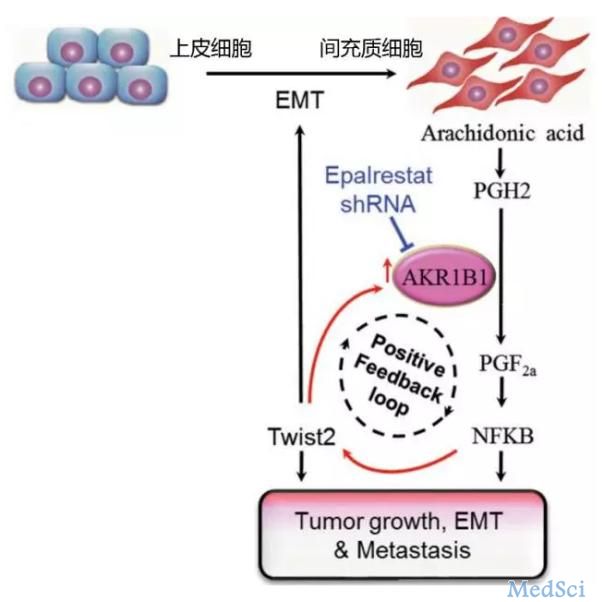
抗内分泌治疗是雌激素受体阳性乳腺癌最有效的治疗方式,但是治疗耐受是临床上常见的并发症。乳腺癌相关成纤维细胞(CAF)是肿瘤微环境中最大的组成部分,在雌激素受体表达以及抗内分泌治疗耐受起到了一定作用。
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#成纤维细胞#
66
#纤维细胞#
63
学习了谢谢分享
83
阅读了谢谢分享。
96
感谢分享一下!
104