Lancet Oncology:前列腺癌筛查,STHLM3模型更靠谱
2015-11-10 Seven L 译 MedSci原创
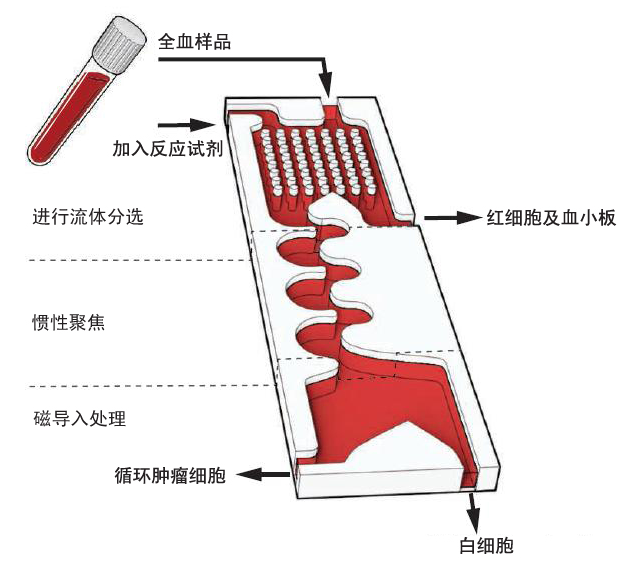
目前临床长常用前列腺特异性抗原 (PSA) 筛查前列腺癌,但是该指标具有很高的假阳性率,会导致不必要的前列腺活检和过度诊断。研究者欲开发和验证一个更好的筛查高危前列腺癌( Gleason得分≥7分)患者的方式。该研究纳入了50-69岁没有前列腺癌的男性。对所有纳入人群检测预定义的STHLM3模型(包括血浆标志物:PSA, free PSA, intact PSA, hK2, MSMB, MIC1;
Henrik Grönberg, Jan Adolfsson, et al.Prostate cancer screening in men aged 50–69 years (STHLM3): a prospective population-based diagnostic study.Lancet Oncology.09 November 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#靠谱#
56
#Lancet#
63
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
98
#Oncol#
52
#Oncology#
63
好好学习
110
好好学习
113
好好学习
90
好好学习
122
好好学习
74