Lancet:预防性输注血小板对成人登革热和血小板患者并无预防出血的益处!
2017-03-13 MedSci MedSci原创
登革热是世界上最常见的媒介传播性传染病之一。它通常与血小板减少相关,因此预防性输注血小板被广泛用于治疗中,但是关于这一疗法仍然缺乏强有力的证据。近期,一项发表在权威杂志Lancet上的研究旨在评估预防性输注血小板在成年登革热和血小板减少症患者中预防出血的功效和安全性。此项研究在新加坡和马来西亚的五家医院进行,为开放标签,随机,优势试验。研究者们招募了21岁及以上的经实验室确诊为登革热(确诊或可能)
登革热是世界上最常见的媒介传播性传染病之一。它通常与血小板减少相关,因此预防性输注血小板被广泛用于治疗中,但是关于这一疗法仍然缺乏强有力的证据。
近期,一项发表在权威杂志Lancet上的研究旨在评估预防性输注血小板在成年登革热和血小板减少症患者中预防出血的功效和安全性。
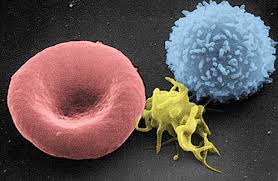
此项研究在新加坡和马来西亚的五家医院进行,为开放标签,随机,优势试验。研究者们招募了21岁及以上的经实验室确诊为登革热(确诊或可能)和血小板减少(血小板≤20000/μL)且无持续性轻度出血或任何严重出血的患者。患者被随机分配(1:1)为支持性护理之外接受预防性血小板输注(输血组)或单独的支持性护理(对照组)。在输血组中,当患者血小板计数为20000/μL或更低时,每天给予4个单位血小板。支持治疗包括卧床休息,液体治疗,发烧和止痛药物。主要研究终点是研究第7天或出院(以较早者为准)的临床出血(不包括瘀点)状况。根据接受的实际治疗分析安全结果。此项研究注册ClinicalTrials.gov,编号NCT01030211。
此项研究结果显示:自2010年4月29日至2014年12月9日,共随机分配372名患者至输血组(n = 188)或对照组(n = 184)。意向性治疗分析包括输血组中的187名患者(一名患者撤出)和182名对照组(其中一名撤出,一名没有确诊或可能的登革热)。
输血组中的40名(21%)患者和对照组中的48名(26%)患者出现第7天或出院时的临床出血(风险差异-4.98%[95%CI -15.08-5.5 34];相对危险度0.81 [95%CI 0.56〜1.17]; p = 0.16)。
输血组发生13例不良事件,对照组发生2例(5.81%[-4.42〜16.01]; 6.26 [1.43〜27.34]; p = 0.0064)。可能或可能与输血有关的不良事件包括三例荨麻疹,一例黄斑丘疹,一例瘙痒和一例胸痛,以及一例过敏反应,一例输血相关的急性肺损伤和一例液体超负荷导致严重的不良事件。没有报告死亡。
此项研究表明,在登革热和血小板减少的成年患者中,预防性输注血小板在预防出血方面并不优于支持性治疗,并且可能与不良事件发生相关。
原始出处:
Lye DC, Archuleta S, et al. Prophylactic platelet transfusion plus supportive care versus supportive care alone in adults with dengue and thrombocytopenia: a multicentre, open-label, randomised, superiority trial. Lancet. 2017 Mar 7. pii: S0140-6736(17)30269-6. doi: 10.1016/S0140-6736(17)30269-6.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#预防性#
67
#Lancet#
91
有趣的研究
102
新药集团好东西!
87
又长见识了。谢谢了
106