Nature Neuroscience:新型化合物保护神经系统发生多发性硬化症的结构损伤
2015-03-02 崔倩译 MedSci原创
根据西奈山伊坎医学院在本周的自然-神经科学杂志在线发表的一项研究,研究显示,在多发性硬化症的小鼠模型中,一个新特征的组的化合物可阻断炎症反应和神经细胞损伤。 多发性硬化症是大脑和脊髓的常见疾病,其原因不明,人体的免疫系统开始发炎攻击对抗髓鞘,保护神经纤维周围的神经涂层。一旦髓鞘从这些纤维剥离,神经细胞变得非常容易受到伤害,这被认为是其背后的破坏,从而导致可见性的多发性硬化症的间进形式,临床稳定性
根据西奈山伊坎医学院在本周的自然-神经科学杂志在线发表的一项研究,研究显示,在多发性硬化症的小鼠模型中,一个新特征的组的化合物可阻断炎症反应和神经细胞损伤。
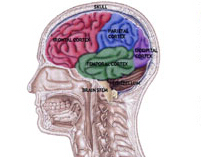
多发性硬化症是大脑和脊髓的常见疾病,其原因不明,人体的免疫系统开始发炎攻击对抗髓鞘,保护神经纤维周围的神经涂层。一旦髓鞘从这些纤维剥离,神经细胞变得非常容易受到伤害,这被认为是其背后的破坏,从而导致可见性的多发性硬化症的间进形式,临床稳定性下降。
该研究的主要作者、西奈山的博士后研究员杰弗里海恩斯博士说:“这项研究中鉴定出的化合物,既减少了多发性硬化的一个标志,即炎症,也保护了小鼠模型中神经细胞受损。目前市场上的多发性硬化症药物正在测试寻求减少对细胞的免疫攻击,但没有目标神经退行性疾病,也没有回复神经细胞功能。这项新研究成果是进一步推进新型口服治疗方案过程中令人振奋的一步。”
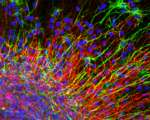
西奈山先前的研究发现,在细胞核(含有细胞的遗传信息的细胞区室)和细胞质之间的蛋白质分子的贩卖在神经变性疾病被改变了。穿梭在细胞核和细胞质的蛋白分子,XPO1(也称为CRM1),和多发性硬化症和许多其它疾病是有牵连的。
具体地讲,西奈山研究的目的是测试药理化合物在表现出一些MS特征的小鼠模型中是否阻止XPO1/ CRM1的功能可以阻止疾病的进展中。研究人员发现,两种化学剂(称为KPT-276和KPT-350)防止XPO1/ CRM1从神经细胞的细胞核流出,该细胞核可以保护它们免受自由基和结构的损伤。这些化合物也停止了炎症细胞繁殖,从而减少炎症。
小
鼠显示在后肢瘫痪后口服KPT-276或KPT-350两周内可恢复运动功能。
该研究的资深作者,神经学、遗传学和基因组学教授帕特里齐亚卡萨西亚博士说:“这项研究结果阐明的多发性硬化症模型疾病的分子机制,为今后的临床试验,以确定与脱髓鞘疾病在人类中这些化学药剂的安全性和有效性提供依据,”
由于核和神经细胞的细胞质之间的分子的流量被改变在几个其它神经变性疾病,靶向核运输可以具有像肌萎缩性侧索硬化症(ALS)和阿耳茨海默氏病的疾病的治疗更广泛的意义。
原始出处
Jeffery D Haines, Olivier Herbin, Belén de la Hera, Oscar G Vidaurre, Gregory A Moy, Qingxiang Sun, Ho Yee Joyce Fung, Stefanie Albrecht, Konstantina Alexandropoulos, Dilara McCauley, Yuh Min Chook, Tanja Kuhlmann, Grahame J Kidd, Sharon Shacham, Patrizia Casaccia. Nuclear export inhibitors avert progression in preclinical models of inflammatory demyelination. Nature Neuroscience, 2015;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#化合物#
45
#Nat#
50
#多发性#
55
#硬化症#
71
#神经系统#
45
#ROS#
67
#SCIE#
81
#损伤#
47
这还仅仅是基础研究而已
146
这还仅仅是基础研究而已
140