Circulation:急性胸痛的更佳评估方法:非侵入性检查 vs. 单纯临床评估
2017-12-11 佚名 国际循环
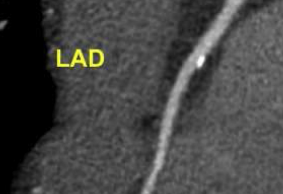
目前,对于急性胸痛的急诊患者,与单纯根据病史、体格检查、心电图及生物标志物行临床评估相比,非侵入性心脏检查(冠脉CT血管造影或负荷试验)与上述临床评估联用能否有助于改善临床结局尚不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#评估方法#
78
#非侵入性#
63
#临床评估#
78
#侵入性#
67
学习了.很好的话题.
86
学习了.涨知识
93
学习了.谢谢分享!
74
学习了很有用
111