Sci Transl Med:摘去肿瘤细胞的“糖衣”,CAR-T即成为“炮弹”!
2022-02-10 生物探索 生物探索
通过基因工程技术将T细胞激活,并装上定位导航到肿瘤的装置-肿瘤嵌合抗原受体(Chimeric Antigen Receptor, CAR),可以将T细胞这个普通“武器”改造成&
通过基因工程技术将T细胞激活,并装上定位导航到肿瘤的装置-肿瘤嵌合抗原受体(Chimeric Antigen Receptor, CAR),可以将T细胞这个普通“武器”改造成“超级武器”,即为CAR-T细胞。CAR-T是治疗B细胞恶性肿瘤的有效疗法,但在实体瘤中疗效有限。这些限制性的因素包括:肿瘤部位T细胞的迁移和浸润不足、抑制信号的持续存在、肿瘤限制性抗原的缺乏。此外,CAR-T疗法的治疗潜力也取决于CAR-T与肿瘤细胞之间形成裂解免疫突触(lytic immune synapse, IS)的形成。
糖基化是最常见的蛋白质修饰之一,产物以糖蛋白的形式出现。糖蛋白是聚糖与蛋白质的天冬酰胺或丝氨酸、苏氨酸残基共价连接而成。与正常细胞相比,肿瘤细胞往往表现出异常的糖基化,形成一种极其多样的细胞外聚糖外衣。这种聚糖外衣可能通过屏蔽免疫细胞的抗原表位或干扰免疫细胞功能,对抗肿瘤反应产生不利影响。b1–6 N-聚糖分支增多是肿瘤细胞最频繁的变异之一,该糖基化修饰是N-乙酰氨基葡萄糖转移酶V(由MGAT5基因编码)活性增加的结果。MGAT5的表达受Ras-Raf-Ets信号通路的正向调控,该通路在肿瘤中通常异常激活,并直接参与肿瘤的生长、侵袭和转移,在多种肿瘤模型中均被证明与生存降低和预后不良相关。
2022年1月19日,来自意大利的研究人员发现多种肿瘤的细胞外N-聚糖表达丰度与CAR-T细胞杀伤程度呈负相关。他们通过敲除胰腺癌(PAC)中的MGAT5发现,N-聚糖能干扰免疫突触形成,减少转录激活、细胞因子和细胞毒性,保护肿瘤免受CAR-T细胞的杀伤。这意味着,一旦破坏肿瘤细胞上的N-聚糖这层“糖衣”,CAR-T细胞活性即得到增强,成为杀伤胰腺癌的重磅“炮弹”。研究成果在线发表于最新一期的Science Translational Medicine(STM)。
研究成果(图源:STM)
为了揭示N-聚糖在胰腺癌中的生物学作用,研究人员首先利用生物信息学数据库分析了参与这些糖基合成的糖基转移酶的突变情况,发现cBioportal的3738名患者中,有19%样本携带参与N-聚糖合成的糖基转移酶的基因组改变,且这一特征与不良预后相关。进一步分析确定仅分支型N-聚糖合成的基因变异与恶化的无病生存显著相关,且大多数变异都是基因扩增。结合TCGA数据库中胰腺癌样本的RNA测序数据的富集分析显示,与健康对照组相比,患者中分支型N-聚糖合成通路显著富集。在富集的基因中,研究者重点关注了分支型N-聚糖生物合成的关键基因MGAT5。
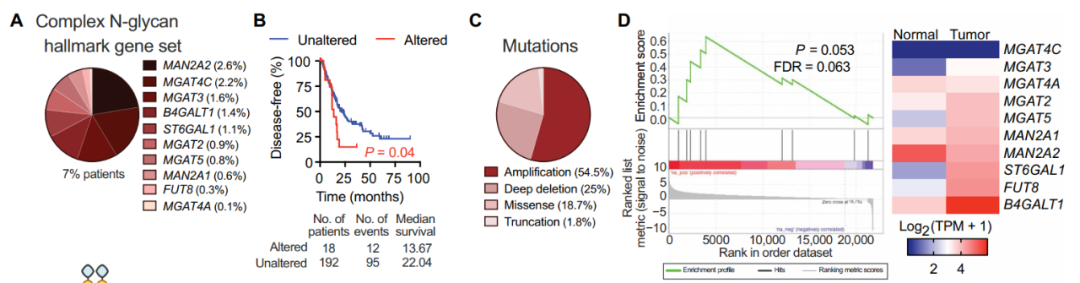
胰腺癌患者的N-聚糖合成相关的基因变异及预后(图源:STM)
敲除MGAT5后发现,CAR-T细胞44v6.28的抗肿瘤效果显著增强,表现为肿瘤细胞溶解活性增加,干扰素和肿瘤坏死因子水平上升。这些结果说明,分支型N-聚糖屏蔽了CAR-T对胰腺癌抗原44v6.28的靶向性。

敲除MGAT5后肿瘤细胞与CAR-T细胞的变化(图源:STM)
为了探明N-聚糖缺陷肿瘤细胞使得抗肿瘤疗效增强的基础,研究者分析了CAR-T细胞靶向过程的限制性步骤——免疫突触IS的形成。结果显示,缺乏MGAT5聚糖产物的胰腺癌细胞与CAR-T44v6.28之间形成了良好的IS,具有更高的F -肌动蛋白积累,更强的颗粒聚合,以及MTOC到F-肌动蛋白的距离缩短,这些是功能性细胞溶解的三个公认参数。对照组细胞中则没有观察到这种差异。该团队还结合Jurkat细胞模型来分析细胞内信号转导事件,也得到与上述一致的结论。这些发现支持了胰腺癌对CAR-T细胞治疗的抵抗机制,即肿瘤接触和CAR-T信号强度受分支型N-聚糖的调控。
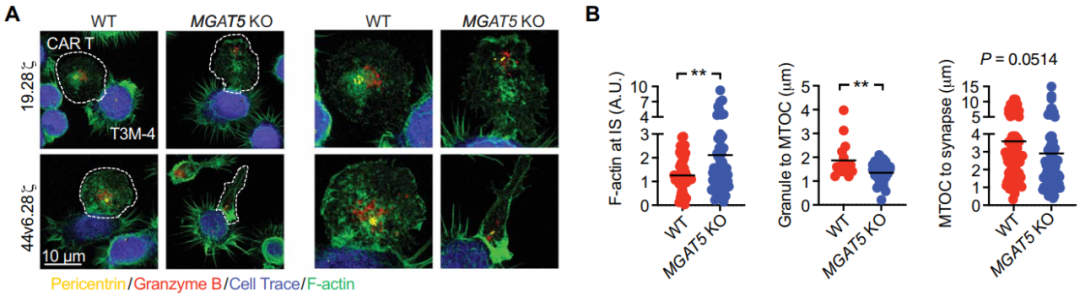
敲除MGAT5后免疫突触与功能性细胞溶解情况(图源:STM)
既然基因层面对N-聚糖的抑制显示出了良好效果,那么从药理学上克服肿瘤糖基化是否也能取得类似效果?研究者巧妙地利用葡萄糖/甘露糖类似物2DG来实现这一干预。2DG此前已被报道能干扰N -链糖基化,合并成新生糖蛋白的脂联寡糖,引起糖基化整体异常状态。研究人员发现,经2DG处理的胰腺癌细胞能被44v6.28细胞更有效地杀死,并在44v6.28细胞中引发了更强的转录作用,但在对照细胞中却没有这种效应。在胰腺癌小鼠异种移植模型中的实验数据显示,无论是低肿瘤负荷、高CAR-T细胞剂量模型,还是高肿瘤负荷、低CAR-T细胞剂量模型,2DG预先注射都能使得肿瘤对CAR-T细胞的攻击更加敏感。此外,该研究还观察到细胞表达抑制性受体的频率显著降低,如T细胞免疫球蛋白域和粘蛋白域3 (TIM-3)、淋巴细胞活化3、程序性细胞死亡蛋白1 (PD-1)和CD57。其中,PD-L1的PD-1相互作用在N-聚糖去除后减弱最为显著。这些发现表明,与2DG联合使用不仅可以提高肿瘤清除能力,还可能使CAR-T细胞避免发生免疫检查点的抑制。
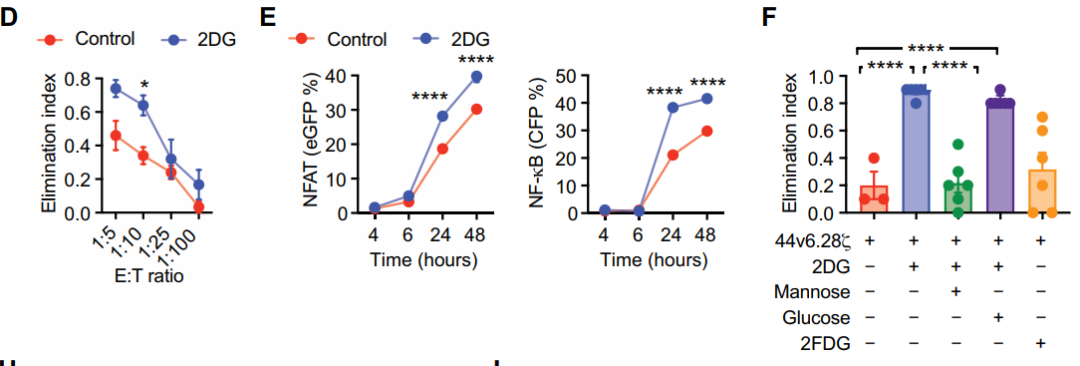
2DG处理后胰腺癌对44v6.28细胞敏感度的影响(图源:STM)
在高肿瘤负荷胰腺癌异种移植小鼠模型中,研究人员比较2DG和44v6.28细胞单独以及组合的长期联合治疗。在T3M-4异种移植模型中,重复注射2DG单独治疗小鼠被证明是无益的,而2DG和44v6.28细胞组合提供了最持久的肿瘤控制,优于两种单独治疗方案。这一结果在BxPC3异种移植模型中亦得到证实。以上结果均表明,与2DG联合治疗可以提高44v6.28细胞的效力并减轻T细胞衰竭。不仅在胰腺癌,研究人员还发现与2DG共同治疗可提高CAR-T细胞对包括膀胱癌和卵巢癌在内的多种肿瘤的治疗效果。
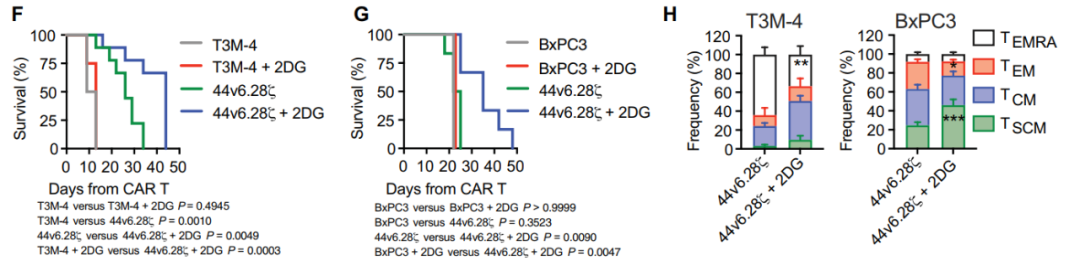
胰腺癌模型中2DG处理、44v6.28细胞治疗的比较(图源:STM)
总之,CAR-T细胞与2DG联合治疗胰腺癌展现出良好的潜力,并且在其他多种肿瘤的治疗中也取得良好效果,包括来自肺、卵巢和膀胱的肿瘤。总的来说,这项研究发现细胞外N-聚糖通过增加CAR-T细胞激活阈值和促进CAR-T细胞衰竭使得肿瘤发生治疗抵抗,也为合理改进实体肿瘤治疗方法提供了新的思路和方向。
参考资料:
[1]Greco B, Malacarne V, De Girardi F, et al. Disrupting N-glycan expression on tumor cells boosts chimeric antigen receptor T cell efficacy against solid malignancies. Sci Transl Med.2022;14(628):eabg3072. doi:10.1126/scitranslmed.abg3072.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
78
#Transl#
105
#CAR-#
62
#肿瘤细胞#
112
#Med#
82
新知识,值得学习
102
#学习#
89
#肿瘤#
101