患者男性,46岁,出现间歇性吞咽固体性食物困难病史1年余。
常规体格检查未见异常。
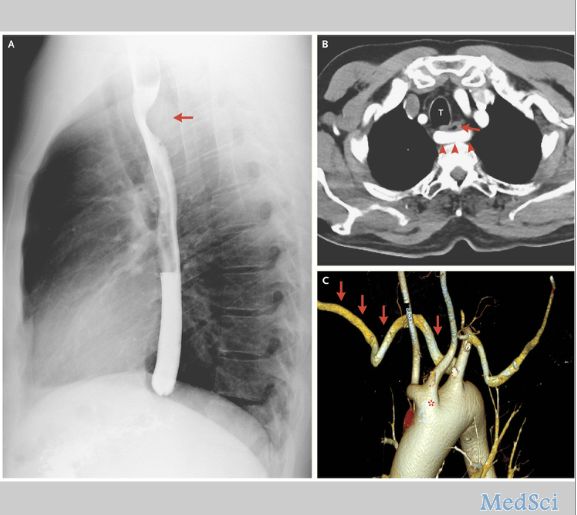
吞钡检查结果显示食管后壁斜向凹陷(如图A箭头处,图B中“T”为食管)。
胸部CT增强扫描显示右锁骨下动脉(图B箭头处;图C为三维重建结构显示),双颈动脉干远端(图C,星号处)和左锁骨下动脉异常。
食管后的右锁骨下动脉异常病变导致食管显著被压缩,这与患者的症状表现是一致的。
由于目前患者吞咽困难只是轻度至中度,拒绝进行手术治疗,最后经血管外科医生会诊后,决定对其保守治疗和改变生活方式来减缓病变的加快。
在临床上,一般情况下患者锁骨下动脉出现病变,通常不表现出任何的症状。当小儿出现锁骨下动脉病变时,有可能会出现反复性地肺部感染或喘鸣,甚至也可能出现吞咽困难现象。
但是,类似于本案例中症状,在成年人中确是比较罕见的。
原始出处:
Bartosz Hudzik, M.D., Ph.D.Mariusz Gąsior, M.D., Ph.D. Dysphagia Lusoria N Engl J Med 2016; 375:e4July 28, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











文章很好值得关注
90
文章很好值得关注
89
不错,提高了临床经验
0
好吧!确实出现吞咽困难不能只说是食管肿瘤
91
文章不错
88
#食管#
56
学习个案,增加经验。
68