JAMA Netw Open:摄入较高的膳食纤维,钙和酸奶可降低结直肠癌发病率
2021-02-19 MedSci原创 MedSci原创
在世界范围内,结直肠癌(CRC)是男性中第三大最常被诊断出的癌症,也是女性第二大最常被诊断出的癌症。CRC的病因是多因素的,其中,遗传因素和环境因素起主要作用。
世界范围内,结直肠癌(CRC)是男性中第三大最常被诊断出的癌症,也是女性第二大最常被诊断出的癌症。CRC的病因是多因素的,其中,遗传因素和环境因素起主要作用。多项研究显示,生活方式在CRC的发生和发展中起重要作用,包括肥胖,不健康饮食和体育锻炼缺乏。
近日,发表在JAMA Netw Open杂志的一项研究显示,摄入较高的膳食纤维,钙和酸奶以及较低的酒精和红肉摄入量可降低CRC的发生风险。
在这项研究中,研究人员检索了MEDLINE、Embase和Cochrane数据库,对222项相关研究进行评估,其中有45项荟萃研究。每项荟萃分析的中位数研究数量为6,中位随访时间为10.2年。中位样本量为598744。中位病例数(即CRC的发生率)为5076例。在这5项已发表的荟萃研究分析中,通过系统评价方法学质量评价工具(AMSTAR-2)对109项饮食因素与CRC发生率之间关系进行风险评估。
结果显示,健康的饮食习惯,地中海饮食,全素食和半素食饮食以及全谷物,总乳制品和补充钙的摄入与CRC发病率呈负相关。红肉和酒精摄入与CRC的发生率呈正相关,而膳食纤维,钙和酸奶的摄入量与CRC的发生呈负相关。

饮食与结直肠癌发病率增加之间关系
具体而言,较高的红肉摄入量与较低的红肉摄入量(AMSTAR-2,高质量)和重度酒精摄入量(AMSTAR-2,中等质量)与CRC发病风险增加相关。相比之下,总膳食纤维(AMSTAR-2,高质量),钙(AMSTAR-2,中等质量)和酸奶(AMSTAR-2,中等质量)的摄入量较高或较低与CRC发病风险降低有关。与较低的摄入量相比,较高的总乳制品摄入量(例如,牛奶,奶酪,酸奶)(AMSTAR-2,高质量)可显着降低CRC风险。但是,与0杯酒或偶尔喝酒相比,适度饮酒(定义为每天>1-3杯但不超过4杯)(AMSTAR-2,中等质量)与CRC发生率增加相关。
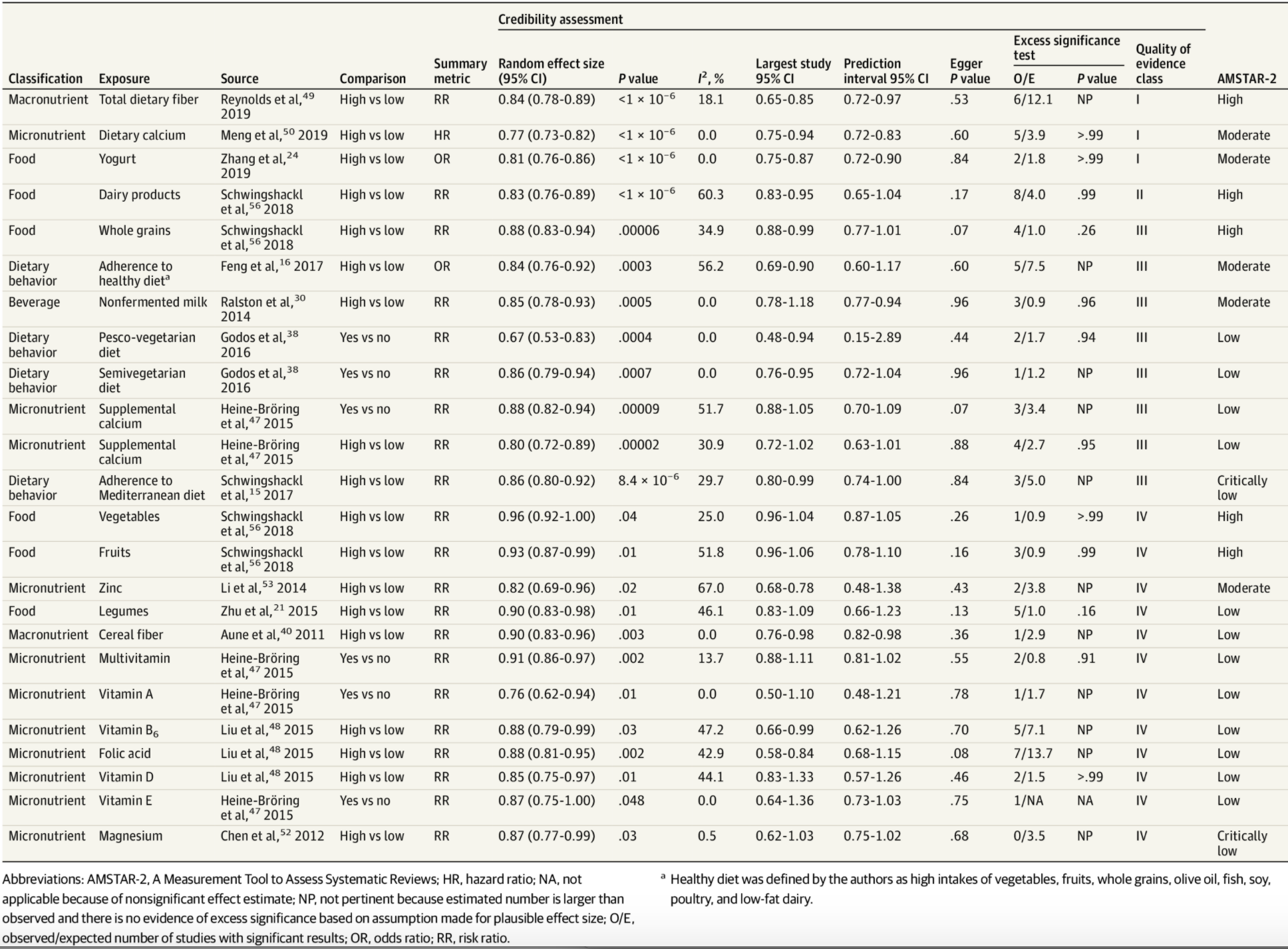
饮食与结直肠癌发病率降低之间关系
另外,饮食或饮食方式与CRC发病风险降低有关,比如,地中海饮食,素食饮食/半素食饮食,全谷物,非发酵乳和补充钙的摄入。然而,也有研究显示,坚持西式饮食和加工肉的摄入与CRC发病风险增加相关。
总之,健康的饮食模式,其特点是摄入较高的蔬菜、水果、全谷物和低脂乳制品的摄入量,较低的酒精和肉制品的摄入量。健康的饮食习惯,地中海饮食,全素食,半素食饮食和半素食饮食以预防CRC,而西方饮食模式则增加CRC风险。
原始出处
Sajesh K. Veettil, PhD1; Tse Yee Wong, B Pharm2; Yee Shen Loo, B Pharm2; et al.Role of Diet in Colorectal Cancer Incidence.Umbrella Review of Meta-analyses of Prospective Observational Studies.JAMA Netw Open. 2021;4(2):e2037341. doi:10.1001/jamanetworkopen.2020.37341
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#NET#
113
#发病率#
118
#PE#
68
#癌发病#
95
#癌发病率#
64
#膳食#
60
#结直肠#
71
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
116