Cell:科学家揭示线粒体应激如何延长线虫寿命
2016-05-24 佚名 生物谷
最近,来自美国加州大学伯克利分校的研究人员在著名国际学术期刊Cell上发表了一项关于线粒体应激促进长寿的最新文章,在这项研究中他们发现线粒体应激能够诱导染色质发生重组,进而促进长寿。 一种生物体的健康状态依赖于对代谢的适应能力,以及能否协调能量需求与营养供应之间的关系。在早期发育阶段急性代谢应激会引起生物体上调一系列保护性基因表达应对应激,并终

最近,来自美国加州大学伯克利分校的研究人员在著名国际学术期刊Cell上发表了一项关于线粒体应激促进长寿的最新文章,在这项研究中他们发现线粒体应激能够诱导染色质发生重组,进而促进长寿。
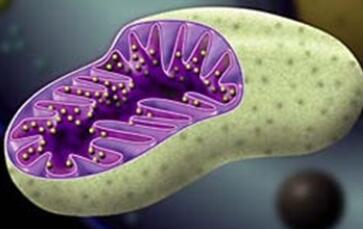
一种生物体的健康状态依赖于对代谢的适应能力,以及能否协调能量需求与营养供应之间的关系。在早期发育阶段急性代谢应激会引起生物体上调一系列保护性基因表达应对应激,并终生保持对代谢功能紊乱的应答,其中还包含了广泛的表观遗传模式变化。线粒体是细胞的代谢中心,之前一些研究表明早期线粒体功能紊乱造成的影响会在生物体内终生存在,比如一项针对多种生物体的研究表明在发育特定阶段温和的线粒体功能紊乱会对寿命带来一定好处。
在这项研究中,研究人员发现线粒体应激会通过组蛋白H3K9二甲基化标记引起染色质结构发生大范围改变,H3K9二甲基化通常与基因沉默有关。对线粒体应激的应答需要组蛋白H3K9发生二甲基化,而这一过程需要组蛋白甲基转移酶met-2以及核内共作用因子lin-65的共同作用才能激活。虽然这些甲基化标记会导致染色质发生全局性基因表达沉默,但是仍有小部分染色质保持开启状态,这些保持开启的位点通常是经典的应激应答因子结合的地方,如DVE-1。
因此,研究人员提出在这样的一种状态下,生物体建立了一种代谢应激应答反应,并保持到动物成年阶段,通过特定的表观遗传修饰允许特定基因表达,并使寿命得到延长。
.
原始出处
Ye Tian, Gilberto Garcia, Qian Bian, Kristan K. Steffen, Larry Joe, Suzanne Wolff, Barbara J. Meyer, Andrew Dillin.Mitochondrial Stress Induces Chromatin Reorganization to Promote Longevity and UPRmt.Cell.2016
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
91
#CEL#
0
#应激#
92
#线虫#
83