一文读懂:胆固醇近期研究亮点
2016-09-15 MedSci MedSci原创
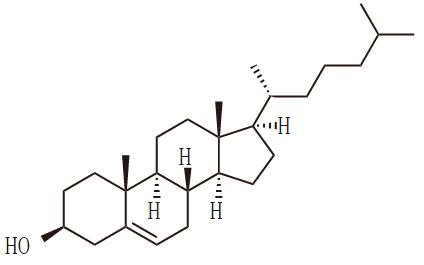
近来,随着美国居民膳食指南取消之前版本中“推荐的每日摄入胆固醇<300 mg/dL”的限制,各种不需限制饮食胆固醇的传言风起云涌,一时间甚嚣尘上。不仅令临床医生困惑,也令广大群众无所适从。那么,到底要不要降脂?为什么需要降低LDL-C?新指南给出了明确答案。2016指南仍将LDL-C视为降低心血管风险的首要靶标,且强调LDL-C降幅越大,心血管风险下降越多;对于极高危患者,LDL-C应尽
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很好的内容,谢谢分享。
90
很好的内容,谢谢分享。
108
继续学习
83
继续关注
0
谢谢分享!
79
继续关注!
42
很好,学习了。
45
学习了,谢谢了
53
学习虚心学习
47